Relationship Between Frailty and Poor Prognosis in Older Trauma Patients in the Emergency Department: A Prospective Cohort Study
-
摘要:目的 探讨衰弱与急诊老年创伤患者不良结局预后的关系。方法 采用前瞻性队列研究设计,纳入2021年1–8月在成都市3所三甲医院急诊科收治的老年创伤患者,按照中文版创伤特异性衰弱指数(Trauma Specific Frailty Index, TSFI)评估结果分为衰弱组和非衰弱组,并记录6个月随访的终点事件(跌倒、再入院和死亡)。采用Cox风险回归模型分析衰弱与急诊老年创伤患者不良结局的关系。结果 共纳入375例急诊老年创伤患者,其中衰弱组131例,非衰弱组244例。随访6个月后,急诊老年创伤患者跌倒、再入院、死亡事件的发生率分别为18.93%、14.40%、7.73%。衰弱组急诊老年创伤患者跌倒(28.24% vs. 13.93%,P=0.001)、再入院(25.95% vs. 8.20%,P=0.000)、死亡(12.98% vs. 4.92%,P=0.005)的发生率均高于非衰弱组。应用Cox风险回归模型调整混杂因素以后,衰弱组发生跌倒〔风险比(hazard ratio, HR)=1.859,95%置信区间(confidence interval, CI):1.070~3.230,P=0.028〕和再入院(HR=2.920,95%CI:1.537~5.547,P=0.001)的风险均高于非衰弱组,衰弱组和非衰弱组发生死亡的风险无明显差异。结论 衰弱是急诊老年创伤患者发生跌倒和再入院的危险因素,衰弱与急诊老年创伤患者发生死亡的风险的相关性需进一步研究。Abstract:Objective To explore the relationship between frailty and adverse outcomes in older trauma patients in the emergency department.Methods A prospective cohort study was conducted. Older trauma patients admitted to the emergency department of three tertiary-care hospitals in Chengdu between January 2021 and August 2021 were enrolled. The patients were divided into a frailty group and a non-frailty group according to their assessment results for Trauma-Specific Frailty Index (TSFI). The end points, including falls, readmission, and deaths, were documented during the 6-month follow-up. Cox risk regression model was used to analyze the relationship between frailty and adverse outcomes in older trauma patients in the emergency department.Results A total of 375 older trauma patients in the emergency department were enrolled, including 131 in the frailty group and 244 in the non-frailty group. After 6 months of follow-up, the incidences of falls, readmission and deaths in older trauma patients in the emergency department were 18.93%, 14.40%, and 7.73%, respectively. The incidences of falls (28.24% vs. 13.93%, P=0.001), readmission (25.95% vs. 8.20%, P=0.000), and deaths (12.98% vs. 4.92%, P=0.005) in older trauma patients in the emergency department in the frailty group were higher than those in the non-frailty group. After adjusting for multiple confounding factors using the Cox regression model, the risks of falls (hazard ratio [HR]=1.859, 95% confidence interval [CI]: 1.070-3.230, P=0.028] and readmission (HR=2.920, 95% CI: 1.537-5.547, P=0.001) were higher in the frailty group than those in the non-frailty group, but there was no significant difference in the risk of deaths between the frailty group and the non-frailty group.Conclusion Frailty is a risk factor for falls and readmissions in older trauma patients in the emergency department and the association between frailty and the risk of deaths in older trauma patients in the emergency department needs to be validated by further studies.
-
Keywords:
- Frailty /
- Emergency department /
- Older adults /
- Trauma /
- Prognosis /
- Prospective cohort study
-
据统计,全球每年约有49%的急诊科老年创伤患者因预后风险被低估而未得到有效的预防和管理[1]。美国创伤外科协会(American Association for Surgery of Trauma, AAST)在《创伤实践管理指南》[2]中提出,对于老年创伤患者的入院评估,不仅应重视对其伤情严重程度的评估,还应重视对其衰弱状态的评估。衰弱是一种生物储备和抗应激反应能力降低的多维临床综合征[3],研究表明,衰弱与促炎细胞因子之间呈正相关,而创伤本就会引起体内促炎性标志物的释放,当衰弱与创伤同时存在时,可加剧创伤后的急性炎症反应,进一步加重老年创伤患者的衰弱状态[4]。国外多项研究[5-6]发现,衰弱状态可导致或加剧急诊老年创伤患者在住院期间出现并发症及死亡等不良预后。随着对衰弱认识水平的不断深入,将衰弱纳入老年创伤患者风险评估和共同决策过程已经逐渐成为共识[5],并提示了解老年患者衰弱与创伤结局之间的关系有助于指导创伤团队启动时进行风险分层、与患者及其家属讨论治疗目标,以及针对老年患者的创伤治疗系统调整和医院资源的调动[7-8]。目前,我国尚缺乏衰弱与急诊老年创伤患者不良结局关系的报告。因此,本研究采用前瞻性队列研究的方法探讨衰弱与我国急诊老年创伤患者不良预后的关系,为我国急诊老年创伤患者的预后风险评估和预防提供参考依据。
1. 对象与方法
1.1 研究对象
本研究是前瞻性队列研究,以方便抽样的方法纳入2021年1–8月于成都市3所三甲医院急诊科就诊的老年创伤患者。纳入标准:①年龄≥60岁;②因外界突发意外(如跌倒、交通事故)造成的机体组织结构完整性被破坏的创伤患者;③创伤后入院时间小于24 h;④自愿参加并签署知情同意书。排除标准:①损伤严重程度评分(Injury Severity Score, ISS)≥25分[9];②入院就诊时临床诊断已经死亡;③入院后因各种原因自主转院或出院。将符合标准的急诊老年创伤患者根据中文版创伤特异性衰弱指数(Trauma-Specific Frailty Index, TSFI)得分分为衰弱组和非衰弱组。最终共纳入375例急诊老年创伤患者,其中衰弱组131例,非衰弱组244例。
本研究经过成都市金牛区人民医院伦理委员会批准通过,批准号QYYLL-2022-011。
1.2 资料收集
1.2.1 基线资料收集
所有研究对象采用标准化的问卷进行基线资料收集,包括研究者自行设计的《一般资料调查表》和ISS调查问卷,资料内容主要为①社会人口学资料,包含:年龄(≥60岁)、性别(男/女)、民族(汉族/其他)、文化程度(初中及以下/初中以上);②一般临床资料,包含:创伤原因(交通/跌倒/其他)、创伤部位(四肢/脑/胸/其他)、是否合并慢性疾病(是/否)、创伤严重程度(ISS<16/ISS≥16)、是否合并院内并发症(是/否)。研究对象的年龄等社会人口学资料通过面对面访谈获得,创伤原因、创伤部位等临床资料通过与医生一同进行体格检查时获得。
1.2.2 衰弱评估
TSFI由美国学者Bellal Josep教授于2014年修订研制,包含15个条目,5个方面(基础疾病、日常活动、身体功能、营养状况和健康态度)[10]。目前广泛应用于创伤老年人衰弱状况评估的相关研究中[11-12]。本研究前期在向Bellal Josep教授获取了英文版TSFI的汉化使用授权后对原版TSFI量表进行了汉化;中文版TSFI Cronbach's α系数为0.861,折半信度为0.698,重测信度为0.871,表示中文版TSFI具有较好的信效度(未发表)。本研究采用中文版TSFI对老年创伤患者的衰弱情况进行评估。TSFI量表每个条目的分数范围从0(代表不衰弱状态)到1(代表严重衰弱状态)。将每个条目得分相加并除以总条目数,总得分介于0~1,TSFI得分<0.25为非衰弱,TSFI得分≥0.25为衰弱。
1.2.3 随访
在完成基线调查后的第6个月通过座机、手机及微信的方式进行随访,记录所有调查对象不良结局情况以及发生时间。若座机/手机及微信通信方式无应答,调查员会寻求医院帮助,查询患者病案,了解其近期是否有就诊情况,尽量收集患者跌倒、再入院、死亡的情况,保证患者随访资料的完整性。其中,死亡为主要终点事件,跌倒及再入院为次要终点事件。失访定义为一次调查中不同日期连续三次无法取得联系或拒绝调查。随访中的失访数据作删失处理,将删失时间和失访前发生的结局事件纳入分析。
1.3 统计学方法
统计分析中计数资料以频数或构成比描述,组间比较采用χ2检验;Kaplan-Meier法绘制生存曲线,并对比例风险(proportional hazards, PH)假定进行检验。log-rank法检验组间不良结局累计发生率的差异;单因素Cox比例风险模型分别纳入年龄、性别、民族、文化水平、创伤原因、创伤部位、ISS评分、有无慢病、有无院内并发症。P<0.05为差异有统计学意义。将单因素分析结果中P<0.1的因素纳入多因素Cox风险回归模型,用以探讨衰弱与急诊老年创伤患者发生不良结局的关系,分别分析衰弱与急诊创伤老年人发生跌倒、再入院以及死亡的风险比(hazard ratio, HR)及其95%置信区间(confidence interval, CI)。为进一步验证结果的稳健性,本研究采用将多因素Cox风险回归模型中的调节因素进行亚组分析的方法进行敏感性分析,同时探究衰弱与不同的分组变量之间是否存在相乘交互作用。
2. 结果
2.1 衰弱组和非衰弱组一般资料比较
本研究共纳入375例急诊老年创伤患者,338例完成了基线调查后的第6个月随访,失访人数37例,失访率9.87%。失访情况如下:4例患者因入住养老机构失去联系;5例患者因随子女移居外地拒绝参加随访;11例患者因对调查内容不感兴趣而不愿参与;17例患者因其他原因拒绝继续参加随访。中文版TSFI评估的衰弱131例(34.93%),非衰弱244例(65.07%)。衰弱组与非衰弱组研究对象的年龄、有无慢性疾病、有无院内并发症之间差异有统计学意义(P<0.001),具体见表1。
表 1 衰弱组和非衰弱组急诊老年创伤患者的一般特征Table 1. General characteristics of frail and non-frail older trauma patients in the emergency departmentCharacteristic Total (n=375) Frail patients (n=131) Non-frail patients (n=244) χ2 P Age/case 27.37 <0.001 60-70 yr. 129 31 98 71-80 yr. 166 53 113 81-90 yr. 80 47 33 Sex/case 0.164 0.685 Men 157 53 104 Women 218 78 140 Ethnicity/case 1.340 0.247 Han Chinese 372 129 243 Others 3 2 1 Highest education attained/case 0.085 0.770 Junior high school or below 208 74 134 Senior high school or above 167 57 110 Cause of trauma/case 0.536 0.765 Traffic accidents 143 47 96 Falls 217 78 139 Others 15 6 9 Location of trauma/case 0.050 0.997 Limbs 226 79 147 Head 74 26 48 Chest 42 15 27 Others 33 11 22 ISS score/case 1.483 0.223 <16 257 95 162 ≥16 118 36 82 Chronic diseases/case 12.188 <0.001 No 169 43 126 Yes 206 88 118 Nosocomial complications/case 85.880 <0.001 Yes 88 67 21 No 287 64 223 2.2 衰弱组和非衰弱组不良结局比较
375例急诊老年创伤患者中,154例在随访期间发生不良结局:跌倒71例,再入院54例,死亡29例。衰弱组和非衰弱组间各不良结局的累积发生率差异均有统计学意义(P<0.05),见表2。
表 2 衰弱组与非衰弱组创伤后6个月不良结局比较Table 2. Comparison of adverse outcomes at 6 months after sustaining trauma between the frail and non-frail patient groupsAdverse outcomes Total
(n=375)Frailty
(n=131)Non-frailty
(n=244)χ2 P Fall/case (%) 71 (18.93) 37 (28.24) 34 (13.93) 11.372 0.001 Readmission/case (%) 54 (14.40) 34 (25.95) 20 (8.19) 21.805 <0.001 Deaths/case (%) 29 (7.73) 17 (12.98) 12 (4.92) 7.759 0.005 2.3 衰弱与急诊老年创伤患者不良结局的关系
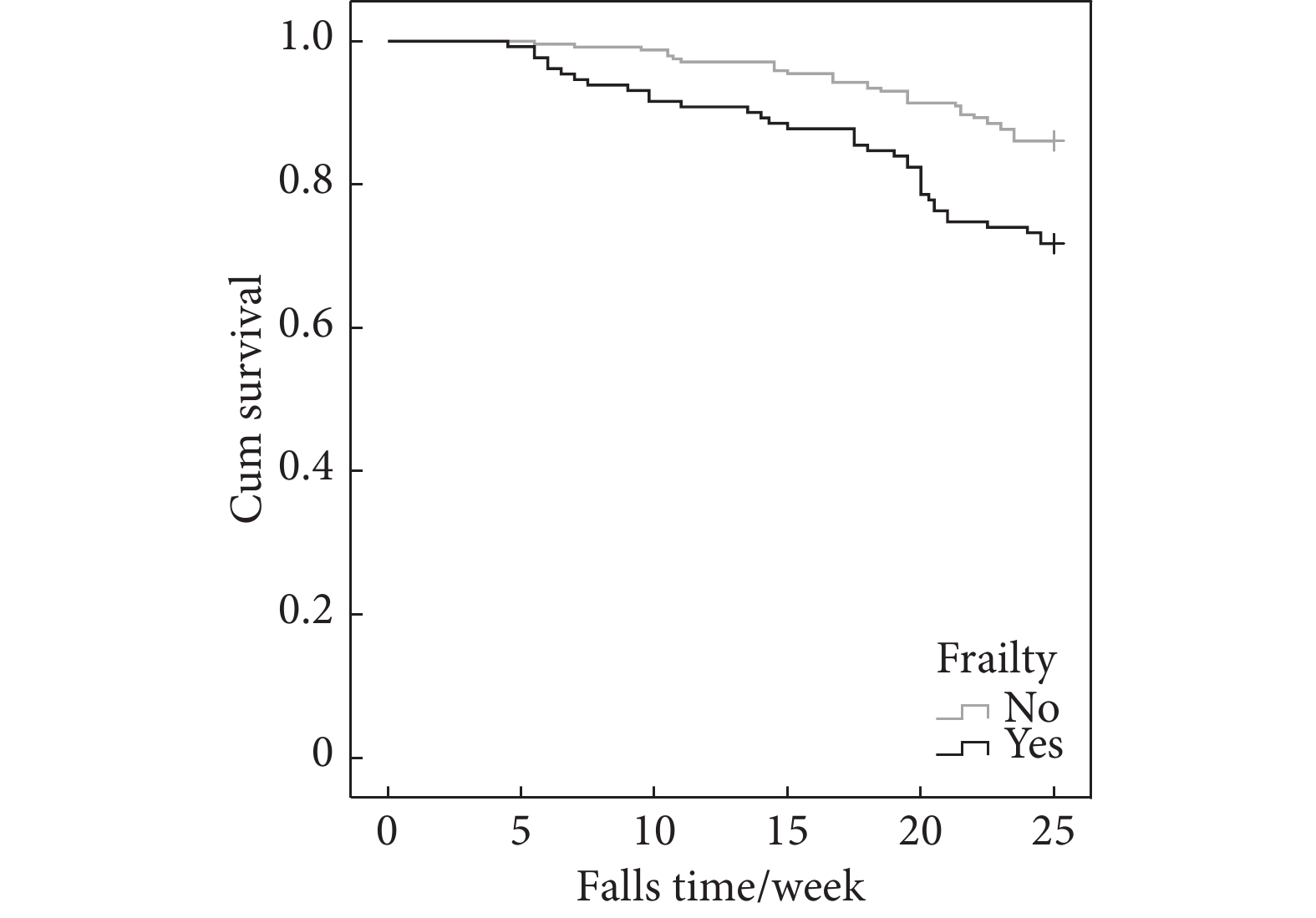
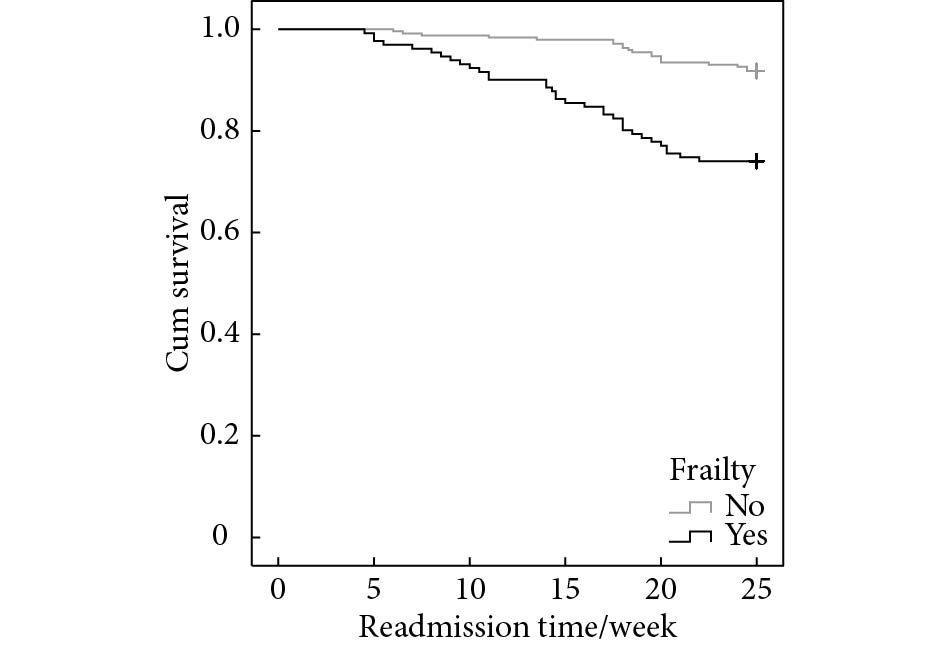
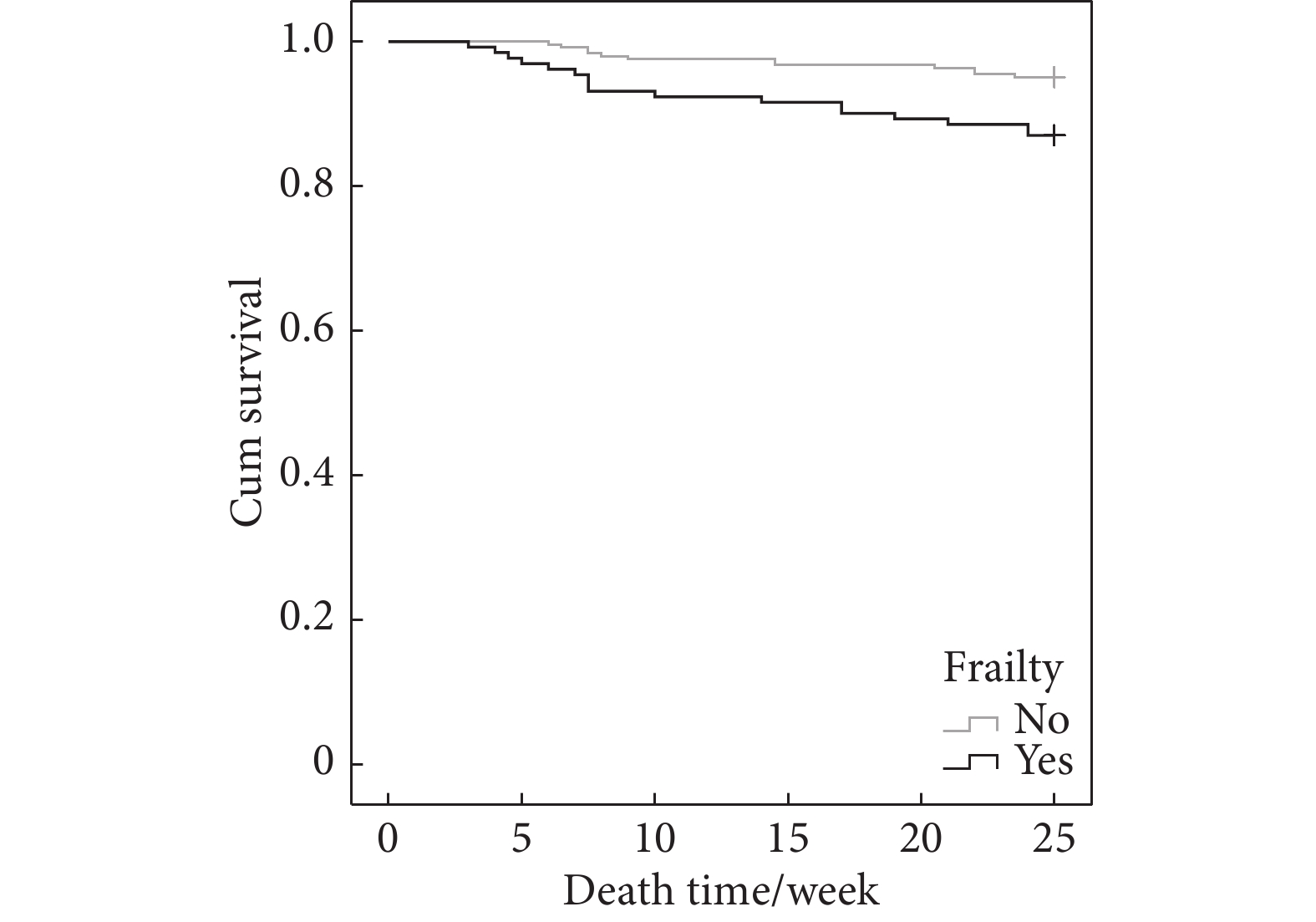
Kaplan-Meier生存分析图显示,衰弱组发生跌倒、再入院及死亡各结局的生存曲线下降程度明显大于非衰弱组。同时,在各不良结局中,衰弱组与非衰弱组的生存曲线不存在交叉,结果均满足PH假定,见图1~图3。log-rank检验显示,衰弱组与非衰弱组在跌倒(χ2=12.350,P<0.001)、再入院(χ2=23.443,P<0.001)及死亡(χ2=7.985,P=0.005)各结局累计发生率的差异均有统计学意义。
2.4 影响急诊老年创伤患者不良结局的单因素Cox回归分析
单因素Cox比例风险回归分析显示,衰弱与急诊老年创伤患者在6个月内跌倒(HR=2.249,95%CI:1.412~3.584,P=0.001)、再入院(HR=3.601,95%CI:2.072~6.258,P<0.001)和死亡(HR=2.771,95%CI:1.323~5.803,P=0.007)的发生相关;年龄与急诊老年创伤患者在6个月内跌倒(HR=1.767,95%CI:1.283~2.435,P<0.001))、再入院(HR=1.814,95%CI:1.259~2.614,P=0.001)和死亡(HR=2.047,95%CI:1.233~3.399,P=0.006)的发生相关;ISS与急诊老年创伤患者在6个月内再入院(HR=2.036,95%CI:1.193~3.477,P=0.009)和死亡(HR=3.808,95%CI:1.798~8.064,P<0.001)的发生相关;有无慢性疾病与急诊老年创伤患者在6个月内跌倒(HR=1.727,95%CI:1.056-2.825,P=0.029)的发生相关;有无院内并发症与急诊老年创伤患者在6个月内跌倒(HR=1.667,95%CI:1.014~2.741,P=0.044)、再入院(HR=3.294,95%CI:1.931~5.620,P<0.001)和死亡(HR=3.698,95%CI:1.785-7.661,P<0.001)的发生相关,见表3。
表 3 单因素Cox比例风险回归分析结果Table 3. Results of the univariate Cox proportional hazards regressionAdverse outcomes Factor β SE Wald χ2 P HR 95% CI Fall Frailty 0.811 0.238 11.636 0.001 2.249 1.412-3.584 Age 0.569 0.163 12.132 <0.001 1.767 1.283-2.435 Sex −0.407 0.254 2.573 0.107 0.666 0.405-1.094 Ethnic group 3.013 5.675 0.282 0.595 20.356 0.000-34.985 Highest education attainment 0.041 0.238 0.029 0.864 1.042 0.653-1.661 Cause of trauma −0.016 0.214 0.005 0.942 0.985 0.647-1.498 Location of trauma −0.010 0.120 0.008 0.931 0.990 0.782-1.253 ISS −0.005 0.257 0.000 0.985 0.995 0.602-1.646 Chronic diseases 0.547 0.251 4.746 0.029 1.727 1.056-2.825 Nosocomial complications 0.511 0.254 4.062 0.044 1.667 1.014-2.741 Readmission Frailty 1.281 0.282 20.649 <0.001 3.601 2.072-6.258 Age 0.595 0.186 10.198 0.001 1.814 1.259-2.614 Sex −0.475 0.293 2.628 0.105 0.622 0.350-1.104 Ethnicity −1.092 1.010 1.171 0.279 0.335 0.046-2.426 Highest education attainment 0.073 0.273 0.071 0.790 1.076 0.630-1.836 Cause of trauma 0.158 0.247 0.410 0.522 1.171 0.722-1.901 Location of trauma 0.039 0.135 0.085 0.771 1.040 0.798-1.355 ISS 0.711 0.273 6.788 0.009 2.036 1.193-3.477 Chronic diseases −0.200 0.272 0.540 0.463 0.819 0.480-1.396 Nosocomial complications 1.192 0.273 19.130 <0.001 3.294 1.931-5.620 Deaths Frailty 1.019 0.377 7.307 0.007 2.771 1.323-5.803 Age 0.716 0.259 7.671 0.006 2.047 1.233-3.399 Sex −0.489 0.401 1.484 0.233 0.613 0.279-1.347 Ethnicity 3.013 9.156 0.108 0.742 20.339 0.000-42.790 Highest education attainment 0.449 0.373 1.445 0.229 1.566 0.753-3.257 Cause of trauma 0.226 0.337 0.447 0.504 1.253 0.647-2.472 Location of trauma 0.176 0.172 1.045 0.307 1.192 0.851-1.670 ISS 1.337 0.383 12.203 <0.001 3.808 1.798-8.064 Chronic diseases −0.432 0.373 1.338 0.247 0.649 0.312-1.350 Nosocomial complications 1.308 0.372 12.382 <0.001 3.698 1.785-7.661 β: regression coefficient; SE: standard error; HR: hazard ratio; CI: confidence interval. 2.5 影响急诊老年创伤患者不良结局的多因素Cox回归分析
在调整混杂因素(年龄、慢性疾病、院内并发症、ISS评分)后,结果发现衰弱仍与急诊老年创伤患者在6个月内跌倒(HR=1.859,95%CI:1.071~3.230,P=0.028)和再入院(HR=1.969,95%CI:1.146~3.382,P=0.014)的发生有关,但与死亡的发生无明显相关性,见表4。
表 4 多因素Cox比例风险回归分析结果Table 4. Results of the multivariate Cox proportional hazards regressionAdverse outcomes Factor β SE Wald χ2 P HR 95% CI Fall Frailty 0.62 0.282 4.844 0.028 1.859 1.070-3.230 Age 0.424 0.333 1.622 0.203 1.528 0.796-2.933 Chronic diseases 0.307 0.26 1.402 0.236 1.36 0.818-2.261 Nosocomial complications −0.147 0.36 0.166 0.684 0.864 0.426-1.749 Readmission Frailty 1.072 0.327 10.716 0.001 2.920 1.537-5.547 Age 0.330 0.193 2.917 0.088 1.390 0.953-2.029 Nosocomialcomplications 0.427 0.334 1.629 0.202 1.532 0.796-2.951 ISS 0.902 0.279 10.445 0.001 2.463 1.426-4.256 Deaths Frailty 0.797 0.426 3.496 0.062 2.219 0.962-5.115 Age 0.769 0.534 2.076 0.150 2.159 0.758-6.149 ISS 1.561 0.398 15.415 <0.001 4.762 2.185-10.38 Nosocomial complications 0.722 0.439 2.703 0.100 2.059 0.87-4.871 β: regression coefficient; SE: standard error; HR: hazard ratio; CI: confidence interval. 2.6 敏感性分析
将研究对象按照不良结局对应的调节变量进行分层,在其余变量均调整的情况下,各不良结局的Cox分析结果如下:①跌倒:在60~69岁、70~79岁、无慢性疾病、无院内并发症的急诊创伤老年患者中,衰弱者更易在创伤后6个月内跌倒(均P<0.05)。②再入院:在70~79岁、≥80岁、无院内并发症、ISS≥16分的急诊创伤老年患者中,衰弱者更易在创伤后6个月内再入院(均P<0.05)。③死亡:在70~79岁、ISS≥16分、无院内并发症的急诊创伤老年患者中,衰弱者更易在创伤后6个月内出现死亡(均P<0.05)。见表5。
表 5 衰弱与急诊创伤老年患者发生不良结局关系的亚组分析和相乘交互作用分析Table 5. Subgroup analysis and multiplicative interaction analysis of the relationship between frailty and adverse outcomes in older trauma patients of the emergency departmentAdverse outcomes Subgroup n Multivariate Cox analysis Pinteractive HR (95% CI) P Fall Age/yr. 0.001 60-69 129 3.875 (1.077, 13.942) 0.038 70-79 166 2.647 (1.288, 5.439) 0.008 ≥80 80 0.844 (0.239, 2.980) 0.792 Chronic diseases 0.073 No 169 3.524 (1.518, 8.178) 0.003 Yes 206 1.188 (0.562, 2.509) 0.652 Nosocomial complications 0.626 No 287 1.747 (1.357, 3.190) 0.049 Yes 88 4.474 (0.845, 23.688) 0.078 Readmission Age/yr. 0.463 60-69 129 0.943 (0.225, 3.950) 0.936 70-79 166 8.349 (3.405, 20.471) <0.001 ≥80 80 13.614 (2.389, 77.294) 0.003 Nosocomial complications <0.001 No 287 9.476 (4.185, 21.456) <0.001 Yes 88 0.416 (0.154, 1.124) 0.084 ISS 0.398 <16 257 1.389 (0.465, 4.145) 0.556 ≥16 118 3.983 (1.720, 9.211) 0.001 Deaths Age/yr. 0.706 60-69 129 0.661 (0.086, 5.059) 0.690 70-79 166 4.479 (1.401, 14.322) 0.011 ≥80 80 3.190 (0.533, 19.083) 0.204 ISS 0.119 <16 257 0.225 (0.038, 1.344) 0.102 ≥16 118 3.587 (1.335, 9.636) 0.011 Nosocomial complications 0.114 No 287 4.166 (1.437, 12.081) 0.009 Yes 88 0.978 (0.267, 3.575) 0.973 HR: hazard ratio; CI: confidence interval. Variables adjusted for each model: falls (age, chronic diseases, nosocomial complications), readmission (age, nosocomial complications, ISS), death (age, nosocomial complications, ISS). 各不良结局的相乘模型结果如下:①跌倒:年龄(P=0.001)与衰弱存在交互作用;②再入院:有无院内并发症(P<0.001)与衰弱存在交互作用;③死亡:无变量与衰弱存在交互作用,见表5。
3. 讨论
TSFI量表是美国学者Bellal Josep教授在50变量的衰弱指数(50-variable frailty index)原量表的基础上修订研制的,针对急性情形下老年创伤患者评估的衰弱量表,更加具有人群场所针对性,信效度良好[10],目前国外已有相关研究[13-14]将该量表用于老年创伤患者的衰弱情况的评估。本研究前期获得了TSFI量表的使用授权并对原版量表进行了汉化和信效度检验,研究结果表明中文版TSFI具有良好的信效度,可用于本研究中急诊创伤老年患者衰弱状态的评估,用以探讨衰弱与急诊创伤老年患者不良预后的关系。
3.1 衰弱对急诊创伤老年患者跌倒的影响
本研究基于前瞻性队列研究探讨了衰弱与急诊创伤老年患者发生跌倒的关系,多因素Cox回归分析结果表明衰弱的急诊创伤老年患者在6个月内更易跌倒。敏感性分析中年龄、有无慢性病、有无院内并发症分组中均有亚组发现衰弱与急诊创伤老年患者发生跌倒有关,进一步证明此研究结果的稳健性较好。
跌倒原本就是急诊老年创伤患者最常见的创伤原因[15],本研究结果进一步表示,衰弱是急诊老年创伤患者发生跌倒的危险因素,跌倒发生率为28.24%,明显高于非衰弱组,与HATCHER等[16]的研究结果相似。说明对于因创伤就诊于急诊的老年患者而言,创伤时是否处于衰弱状态显著影响其在随访期间跌倒的发生情况。从生理方面来讲,处于衰弱状态的老年人,由于生理储备能力降低,肌纤维萎缩、骨量减少、肌力下降导致维持自身稳态的能力下降[17],与此同时,创伤的应激状态下,促炎因子水平的提高进一步加剧了老年患者的炎症水平,导致肌肉蛋白质降解,肌肉力量的减退增加了跌倒的可能[18-19]。从心理方面来讲,创伤老年患者跌倒的发生可能与跌倒恐惧(fear of falling, FOF)有关。研究表明,发生过跌倒的老年人中40%以上存在FOF的心理障碍,而衰弱老年人跌倒后FOF的发生率更高[20]。衰弱的创伤老年人由于担心跌倒的不良影响,在身体机能衰退的情况下进一步减少了身体活动,导致肌肉质量的降低和肌肉力量的损失,不仅对身体平衡等功能产生了影响,并且加剧了营养不良、焦虑和抑郁程度,从生理和心理方面都加重了其衰弱程度,再次跌倒的风险也随之增加[4,21-22]。因此急诊医护人员应加强对老年创伤患者衰弱情况的评估,重视对患者的健康教育,缓解因FOF等造成的负性情绪体验,降低衰弱老年创伤患者跌倒的发生率。
3.2 衰弱对急诊创伤老年患者再入院的影响
本研究结果显示衰弱是急诊创伤老年患者6个月内再入院的危险因素,敏感性分析中年龄、有无院内并发症、ISS分组中均有亚组发现衰弱与急诊创伤老年患者发生再入院有关,进一步证明此研究结果的稳健性较好。与诸多的研究[23-24]结果相似,认为衰弱是创伤老年患者发生再入院结局事件的重要预测因素。但也有研究认为,衰弱与老年创伤患者再入院之间无明显关系[25]。这种差异可能是由于研究之间纳入和排除标准以及使用的衰弱评估工具不同所致。有研究[26]证明营养不良的衰弱患者由于白蛋白下降造成代谢紊乱,引起机体免疫力降低、炎症反应增加,相较于健康老年人,存在更高再入院风险。HATCHER等[16]的研究进一步表明,与非衰弱患者相比,有跌倒史的衰弱患者再入院的百分比更高。分析其原因可能在于:衰弱老年患者因为营养不良等因素对疾病的易感性增加、承受内部和外部应激压力的能力受损[27],在对抗应激源的能力、自身的修复功能处于代偿失调的状态下,创伤作为外界应激导致身体炎症产物增加,由于对压力的过度分解和过度代谢反应,使得急性期蛋白质进一步减少,也使其更易发生创伤后再入院的不良结局[28]。因此对于急诊创伤的老年患者,除了及时评估衰弱状态以外,医护人员应重视对其营养状态的评估,对于营养不良的情况应给予积极纠正,防止因为营养缺乏增加衰弱创伤患者再入院的风险。
3.3 衰弱对急诊创伤老年患者死亡的影响
本研究分析随访6个月结果发现,急诊老年创伤患者中衰弱组死亡结局的发生率明显高于非衰弱组,衰弱组与非衰弱组的死亡结局事件累计发生率也存在显著差异。但通过多因素Cox风险回归分析对混杂因素年龄、院内并发症、ISS矫正后,衰弱与急诊老年创伤患者6个月内死亡结局事件相关不明显。敏感性分析中年龄、ISS、有无院内并发症分组中也均有亚组发现衰弱与急诊创伤老年患者发生死亡有关。这可能与发生死亡这一不良结局的样本量较少有关。在CURTIS等[29]的研究中,衰弱的急诊老年创伤患者比非衰弱患者存在更高的死亡风险(OR=1.52,95%CI:1.37~1.69),与本研究结果不相一致。分析其中原因,可能是因为该研究是对2年内急诊创伤老年人的不良结局的发生情况进行观察,研究时间相对较长,而本研究随访时间较短,只观察到了长期死亡率的一部分,未来可延长随访时间,对研究结果进行进一步的验证。研究证实并强调失能、死亡是急诊老年创伤患者非常易出现的严重不良结局,对合并衰弱等高风险的患者进行预防管理可以降低不良结局的发生概率,因此在未来的研究中需要重视衰弱对创伤老年患者发生死亡等严重不良结局的早期识别和干预[5]。
最近一项国际范围审查报告指出,在急诊科对具有衰弱或衰弱风险的创伤患者进行识别的护理阶段,仅有14%的患者进行了衰弱筛查[30]。鉴于急诊老年创伤患者衰弱的高发率及导致的严重不良结局,临床实践中加强对这一方面的关注,进行及时准确的检测并进行有效的干预是非常有必要的。对此,本研究提出以下建议:首先,应该选择切实有效的评估工具对急诊创伤老年患者的衰弱状态进行评估。目前,衰弱评估工具的数量较多,各工具对衰弱的识别能力尚缺乏较为统一的共识,在未来的研究中可进一步开展衰弱工具对创伤老年患者不良结局的预测能力比较,为创伤老年患者衰弱的识别提供更为准确的评估工具;其次,改善个体衰弱创伤患者的护理策略,提高对相关风险的认识,并优化衰弱患者的医疗保健系统至关重要。例如,加强老年护理过程,强调早期康复可以潜在地降低并发症和功能丧失的风险;此外,以老年人为中心的创伤病房[31]和针对创伤患者的综合老年医学咨询[32]已经在特定领域(如减少多种药物/高风险药物的使用)显示出可能有益的信号,以早期出院为导向的护理计划已经在老年外科患者的护理中体现出了相应的优势[33],以上均可为老年创伤患者衰弱的有效识别和管理提供新的思路。
本研究仍存在不足之处:①样本代表性和随访时间:本研究仅选择了3所医院急诊科的老年创伤患者作为调查对象,随访时间相对较短,可能会对研究结果产生一定影响,未来可进一步开展多中心的大样本调查,延长随访时间,对研究结果进行进一步的验证;②随访信息偏差:本研究采用电话/微信进行随访,受随访方式的影响,对于随访信息的收集可能存在一定的偏差。
综上,本研究前瞻性地分析了衰弱与我国急诊创伤老年患者发生跌倒、再入院、死亡不良结局的关系,结果表明衰弱是急诊创伤老年患者发生跌倒、再入院的危险因素,可能与急诊创伤老年患者死亡的发生有关。此结论提示对于因创伤就诊于急诊科的老年人,医护人员应加强对其衰弱情况的评估,对于衰弱水平较高的患者采取积极有效的干预方案以降低老年创伤患者不良结局的发生率。
* * *
作者贡献声明 杨静负责论文构思,杨静和陈昕羽负责数据审编和初稿写作,杨静、陈昕羽和柏丁兮负责正式分析和调查研究,高静负责经费获取、提供资源、监督指导和审读与编辑写作,杨静、柏丁兮和吴晨曦负责研究方法,吴晨曦负责研究项目管理、软件和可视化,柏丁兮负责验证。所有作者已经同意将文章提交给本刊,且对将要发表的版本进行最终定稿,并同意对工作的所有方面负责。
利益冲突 所有作者均声明不存在利益冲突
-
表 1 衰弱组和非衰弱组急诊老年创伤患者的一般特征
Table 1 General characteristics of frail and non-frail older trauma patients in the emergency department
Characteristic Total (n=375) Frail patients (n=131) Non-frail patients (n=244) χ2 P Age/case 27.37 <0.001 60-70 yr. 129 31 98 71-80 yr. 166 53 113 81-90 yr. 80 47 33 Sex/case 0.164 0.685 Men 157 53 104 Women 218 78 140 Ethnicity/case 1.340 0.247 Han Chinese 372 129 243 Others 3 2 1 Highest education attained/case 0.085 0.770 Junior high school or below 208 74 134 Senior high school or above 167 57 110 Cause of trauma/case 0.536 0.765 Traffic accidents 143 47 96 Falls 217 78 139 Others 15 6 9 Location of trauma/case 0.050 0.997 Limbs 226 79 147 Head 74 26 48 Chest 42 15 27 Others 33 11 22 ISS score/case 1.483 0.223 <16 257 95 162 ≥16 118 36 82 Chronic diseases/case 12.188 <0.001 No 169 43 126 Yes 206 88 118 Nosocomial complications/case 85.880 <0.001 Yes 88 67 21 No 287 64 223 表 2 衰弱组与非衰弱组创伤后6个月不良结局比较
Table 2 Comparison of adverse outcomes at 6 months after sustaining trauma between the frail and non-frail patient groups
Adverse outcomes Total
(n=375)Frailty
(n=131)Non-frailty
(n=244)χ2 P Fall/case (%) 71 (18.93) 37 (28.24) 34 (13.93) 11.372 0.001 Readmission/case (%) 54 (14.40) 34 (25.95) 20 (8.19) 21.805 <0.001 Deaths/case (%) 29 (7.73) 17 (12.98) 12 (4.92) 7.759 0.005 表 3 单因素Cox比例风险回归分析结果
Table 3 Results of the univariate Cox proportional hazards regression
Adverse outcomes Factor β SE Wald χ2 P HR 95% CI Fall Frailty 0.811 0.238 11.636 0.001 2.249 1.412-3.584 Age 0.569 0.163 12.132 <0.001 1.767 1.283-2.435 Sex −0.407 0.254 2.573 0.107 0.666 0.405-1.094 Ethnic group 3.013 5.675 0.282 0.595 20.356 0.000-34.985 Highest education attainment 0.041 0.238 0.029 0.864 1.042 0.653-1.661 Cause of trauma −0.016 0.214 0.005 0.942 0.985 0.647-1.498 Location of trauma −0.010 0.120 0.008 0.931 0.990 0.782-1.253 ISS −0.005 0.257 0.000 0.985 0.995 0.602-1.646 Chronic diseases 0.547 0.251 4.746 0.029 1.727 1.056-2.825 Nosocomial complications 0.511 0.254 4.062 0.044 1.667 1.014-2.741 Readmission Frailty 1.281 0.282 20.649 <0.001 3.601 2.072-6.258 Age 0.595 0.186 10.198 0.001 1.814 1.259-2.614 Sex −0.475 0.293 2.628 0.105 0.622 0.350-1.104 Ethnicity −1.092 1.010 1.171 0.279 0.335 0.046-2.426 Highest education attainment 0.073 0.273 0.071 0.790 1.076 0.630-1.836 Cause of trauma 0.158 0.247 0.410 0.522 1.171 0.722-1.901 Location of trauma 0.039 0.135 0.085 0.771 1.040 0.798-1.355 ISS 0.711 0.273 6.788 0.009 2.036 1.193-3.477 Chronic diseases −0.200 0.272 0.540 0.463 0.819 0.480-1.396 Nosocomial complications 1.192 0.273 19.130 <0.001 3.294 1.931-5.620 Deaths Frailty 1.019 0.377 7.307 0.007 2.771 1.323-5.803 Age 0.716 0.259 7.671 0.006 2.047 1.233-3.399 Sex −0.489 0.401 1.484 0.233 0.613 0.279-1.347 Ethnicity 3.013 9.156 0.108 0.742 20.339 0.000-42.790 Highest education attainment 0.449 0.373 1.445 0.229 1.566 0.753-3.257 Cause of trauma 0.226 0.337 0.447 0.504 1.253 0.647-2.472 Location of trauma 0.176 0.172 1.045 0.307 1.192 0.851-1.670 ISS 1.337 0.383 12.203 <0.001 3.808 1.798-8.064 Chronic diseases −0.432 0.373 1.338 0.247 0.649 0.312-1.350 Nosocomial complications 1.308 0.372 12.382 <0.001 3.698 1.785-7.661 β: regression coefficient; SE: standard error; HR: hazard ratio; CI: confidence interval. 表 4 多因素Cox比例风险回归分析结果
Table 4 Results of the multivariate Cox proportional hazards regression
Adverse outcomes Factor β SE Wald χ2 P HR 95% CI Fall Frailty 0.62 0.282 4.844 0.028 1.859 1.070-3.230 Age 0.424 0.333 1.622 0.203 1.528 0.796-2.933 Chronic diseases 0.307 0.26 1.402 0.236 1.36 0.818-2.261 Nosocomial complications −0.147 0.36 0.166 0.684 0.864 0.426-1.749 Readmission Frailty 1.072 0.327 10.716 0.001 2.920 1.537-5.547 Age 0.330 0.193 2.917 0.088 1.390 0.953-2.029 Nosocomialcomplications 0.427 0.334 1.629 0.202 1.532 0.796-2.951 ISS 0.902 0.279 10.445 0.001 2.463 1.426-4.256 Deaths Frailty 0.797 0.426 3.496 0.062 2.219 0.962-5.115 Age 0.769 0.534 2.076 0.150 2.159 0.758-6.149 ISS 1.561 0.398 15.415 <0.001 4.762 2.185-10.38 Nosocomial complications 0.722 0.439 2.703 0.100 2.059 0.87-4.871 β: regression coefficient; SE: standard error; HR: hazard ratio; CI: confidence interval. 表 5 衰弱与急诊创伤老年患者发生不良结局关系的亚组分析和相乘交互作用分析
Table 5 Subgroup analysis and multiplicative interaction analysis of the relationship between frailty and adverse outcomes in older trauma patients of the emergency department
Adverse outcomes Subgroup n Multivariate Cox analysis Pinteractive HR (95% CI) P Fall Age/yr. 0.001 60-69 129 3.875 (1.077, 13.942) 0.038 70-79 166 2.647 (1.288, 5.439) 0.008 ≥80 80 0.844 (0.239, 2.980) 0.792 Chronic diseases 0.073 No 169 3.524 (1.518, 8.178) 0.003 Yes 206 1.188 (0.562, 2.509) 0.652 Nosocomial complications 0.626 No 287 1.747 (1.357, 3.190) 0.049 Yes 88 4.474 (0.845, 23.688) 0.078 Readmission Age/yr. 0.463 60-69 129 0.943 (0.225, 3.950) 0.936 70-79 166 8.349 (3.405, 20.471) <0.001 ≥80 80 13.614 (2.389, 77.294) 0.003 Nosocomial complications <0.001 No 287 9.476 (4.185, 21.456) <0.001 Yes 88 0.416 (0.154, 1.124) 0.084 ISS 0.398 <16 257 1.389 (0.465, 4.145) 0.556 ≥16 118 3.983 (1.720, 9.211) 0.001 Deaths Age/yr. 0.706 60-69 129 0.661 (0.086, 5.059) 0.690 70-79 166 4.479 (1.401, 14.322) 0.011 ≥80 80 3.190 (0.533, 19.083) 0.204 ISS 0.119 <16 257 0.225 (0.038, 1.344) 0.102 ≥16 118 3.587 (1.335, 9.636) 0.011 Nosocomial complications 0.114 No 287 4.166 (1.437, 12.081) 0.009 Yes 88 0.978 (0.267, 3.575) 0.973 HR: hazard ratio; CI: confidence interval. Variables adjusted for each model: falls (age, chronic diseases, nosocomial complications), readmission (age, nosocomial complications, ISS), death (age, nosocomial complications, ISS). -
[1] GIROUX M, SIROIS M J, BOUCHER V, et al. Frailty assessment to help predict patients at risk of delirium when consulting the emergency department. J Emerg Med,2018,55(2): 157–164. DOI: 10.1016/j.jemermed.2018.02.032
[2] CALLAND J F, INGRAHAM A M, MARTIN N, et al. Evaluation and management of geriatric trauma: an Eastern Association for the surgery of trauma practice management guideline. J Trauma Acute Care Surg,2012,73(5 Suppl 4): S345–S350. DOI: 10.1097/TA.0b013e318270191f
[3] 谢玉磊, 沈炼伟, 胡安丽, 等. 中老年人衰弱综合征危险因素分析及列线图预测模型的构建. 现代预防医学,2022,49(24): 4430–4436. DOI: 10.20043/j.cnki.MPM.202204413 [4] PALMER J, PANDIT V, ZEESHAN M, et al. The acute inflammatory response after trauma is heightened by frailty: a prospective evaluation of inflammatory and endocrine system alterations in frailty. J Trauma Acute Care Surg,2019,87(1): 54–60. DOI: 10.1097/TA.0000000000002229
[5] CHEUNG A, HAAS B, RINGER T J, et al. Canadian study of health and aging clinical frailty scale: does it predict adverse outcomes among geriatric trauma patients? J Am Coll Surg,2017,225(5): 658–665.e3. DOI: 10.1016/j.jamcollsurg.2017.08.008
[6] JOSEPH B, PANDIT V, ZANGBAR B, et al. Superiority of frailty over age in predicting outcomes among geriatric trauma patients: a prospective analysis. JAMA Surg,2014,149(8): 766–772. DOI: 10.1001/jamasurg.2014.296
[7] MAXWELL C A, MION L C, MUKHERJEE K, et al. Preinjury physical frailty and cognitive impairment among geriatric trauma patients determine postinjury functional recovery and survival. J Trauma Acute Care Surg,2016,80(2): 195–203. DOI: 10.1097/TA.0000000000000929
[8] POULTON A, SHAW J F, NGUYEN F, et al. The association of frailty with adverse outcomes after multisystem trauma: a systematic review and meta-analysis. Anesth Analg,2020,130(6): 1482–1492. DOI: 10.1213/ANE.0000000000004687
[9] 杨超, 张旭, 李潭, 等. 创伤严重程度评分对多发创伤患者深静脉血栓形成的预测价值. 实用医学杂志,2021,37(18): 2371–2374. DOI: 10.3969/j.issn.1006-5725.2021.18.013 [10] JOSEPH B, PANDIT V, ZANGBAR B, et al. Validating trauma-specific frailty index for geriatric trauma patients: a prospective analysis. J Am Coll Surg,2014,219(1): 10–17.e1. DOI: 10.1016/j.jamcollsurg.2014.03.020
[11] HAMIDI M, ZEESHAN M, O'KEEFFE T, et al. Prospective evaluation of frailty and functional independence in older adult trauma patients. Am J Surg,2018,216(6): 1070–1075. DOI: 10.1016/j.amjsurg.2018.10.023
[12] MCCUSKER A, KHAN M, KULVATUNYOU N, et al. Sarcopenia defined by a computed tomography estimate of the psoas muscle area does not predict frailty in geriatric trauma patients. Am J Surg,2019,218(2): 261–265. DOI: 10.1016/j.amjsurg.2018.07.024
[13] JARMAN H, CROUCH R, BAXTER M, et al. Feasibility and accuracy of ED frailty identification in older trauma patients: a prospective multi-centre study. Scand J Trauma Resusc Emerg Med,2021,29(1): 54. DOI: 10.1186/s13049-021-00868-4
[14] JOSEPH B, SALJUQI A T, AMOS J D, et al. Prospective validation and application of the Trauma-Specific Frailty Index: results of an American Association for the Surgery of Trauma multi-institutional observational trial. J Trauma Acute Care Surg,2023,94(1): 36–44. DOI: 10.1097/TA.0000000000003817
[15] MORELAND B, KAKARA R, HENRY A. Trends in nonfatal falls and fall-related injuries among adults aged ≥65 years--United States, 2012-2018. MMWR Morb Mortal Wkly Rep,2020,69(27): 875–881. DOI: 10.15585/mmwr.mm6927a5
[16] HATCHER V H, GALET C, LILIENTHAL M, et al. Association of clinical frailty scores with hospital readmission for falls after index admission for trauma-related injury. JAMA Netw Open,2019,2(10): e1912409. DOI: 10.1001/jamanetworkopen.2019.12409
[17] 李丽君, 刘丽华, 陈小玲, 等. 渐进式抗阻运动对养老机构衰弱老年人的影响. 护理学杂志,2022,37(22): 90–93. DOI: 10.3870/j.issn.1001-4152.2022.22.090 [18] SOYSAL P, STUBBS B, LUCATO P, et al. Inflammation and frailty in the elderly: a systematic review and meta-analysis. Ageing Res Rev,2016,31: 1–8. DOI: 10.1016/j.arr.2016.08.006
[19] De SOUZA L F, CANEVER J B, MOREIRA B S, et al. Association between fear of falling and frailty in community-dwelling older adults: a systematic review. Clin Interv Aging,2022,17: 129–140. DOI: 10.2147/CIA.S328423
[20] MERCHANT R A, CHEN M Z, WONG B L L, et al. Relationship between fear of falling, fear-related activity restriction, frailty, and sarcopenia. J Am Geriatr Soc,2020,68(11): 2602–2608. DOI: 10.1111/jgs.16719
[21] 中华医学会老年医学分会. 老年患者衰弱评估与干预中国专家共识. 中华老年医学杂志,2017,36(3): 251–256. DOI: 10.3760/cma.j.issn.0254-9026.2017.03.007 [22] MÖRS K, WAGNER N, STURM R, et al. Enhanced pro-inflammatory response and higher mortality rates in geriatric trauma patients. Eur J Trauma Emerg Surg,2021,47(4): 1065–1072. DOI: 10.1007/s00068-019-01284-1
[23] WAHL T S, GRAHAM L A, HAWN M T, et al. Association of the modified frailty index with 30-day surgical readmission. JAMA Surg,2017,152(8): 749–757. DOI: 10.1001/jamasurg.2017.1025
[24] ENGELHARDT K E, REUTER Q, LIU J, et al. Frailty screening and a frailty pathway decrease length of stay, loss of independence, and 30-day readmission rates in frail geriatric trauma and emergency general surgery patients. J Trauma Acute Care Surg,2018,85(1): 167–173. DOI: 10.1097/TA.0000000000001931
[25] CHUA X Y, TOH S, WEI K, et al. Evaluation of clinical frailty screening in geriatric acute care. J Eval Clin Pract,2020,26(1): 35–41. DOI: 10.1111/jep.13096
[26] RASHIDI POUR FARD N, AMIRABDOLLAHIAN F, HAGHIGHATDOOST F. Dietary patterns and frailty: a systematic review and meta-analysis. Nutr Rev,2019,77(7): 498–513. DOI: 10.1093/nutrit/nuz007
[27] FRIED L P, FERRUCCI L, DARER J, et al. Untangling the concepts of disability, frailty, and comorbidity: implications for improved targeting and care. J Gerontol A Biol Sci Med Sci,2004,59(3): 255–263. DOI: 10.1093/gerona/59.3.m255
[28] ERNST A, WILSON J M, AHN J, et al. Malnutrition and the orthopaedic trauma patient: a systematic review of the literature. J Orthop Trauma,2018,32(10): 491–499. DOI: 10.1097/BOT.0000000000001254
[29] CURTIS E, ROMANOWSKI K, SEN S, et al. Frailty score on admission predicts mortality and discharge disposition in elderly trauma patients over the age of 65 y. J Surg Res,2018,230: 13–19. DOI: 10.1016/j.jss.2018.04.017
[30] THEOU O, SQUIRES E, MALLERY K, et al. What do we know about frailty in the acute care setting? A scoping review. BMC Geriatr,2018,18(1): 139. DOI: 10.1186/s12877-018-0823-2
[31] MANGRAM A J, MITCHELL C D, SHIFFLETTE V K, et al. Geriatric trauma service: a one-year experience. J Trauma Acute Care Surg,2012,72(1): 119–122. DOI: 10.1097/TA.0b013e318241f0ba
[32] SHARMA J, PARULEKAR M, STEWART P, et al. Geriatric consultation reduces high-risk medication usage at discharge in elderly trauma patients. Cureus,2018,10(11): e3649. DOI: 10.7759/cureus.3649
[33] MCDONALD S R, HEFLIN M T, WHITSON H E, et al. Association of integrated care coordination with postsurgical outcomes in high-risk older adults: the perioperative optimization of senior health (POSH) initiative. JAMA Surg,2018,153(5): 454–462. DOI: 10.1001/jamasurg.2017.5513
-
期刊类型引用(2)
1. 高悦,陈可,蒋丹丹,佘柯仪,张红涛,阳欣君,张雯,周雨彤,陈尧,尹心红. 老年急诊创伤患者衰弱现状及其危险因素. 临床与病理杂志. 2025(01): 46-54 .  百度学术
百度学术
2. 袁美玲,刘霞,赵林,脱淼,杨海朋,魏丽丽. 近10年国内外老年急诊护理研究的可视化分析. 循证护理. 2024(19): 3541-3546 .  百度学术
百度学术
其他类型引用(2)

开放获取 本文遵循知识共享署名—非商业性使用4.0国际许可协议(CC BY-NC 4.0),允许第三方对本刊发表的论文自由共享(即在任何媒介以任何形式复制、发行原文)、演绎(即修改、转换或以原文为基础进行创作),必须给出适当的署名,提供指向本文许可协议的链接,同时标明是否对原文作了修改;不得将本文用于商业目的。CC BY-NC 4.0许可协议详情请访问 https://creativecommons.org/licenses/by-nc/4.0

 首页
首页


 下载:
下载: