Clinical Comparative Analysis of Early-Onset Preeclampsia Combined with HELLP Syndrome
-
摘要:目的 探讨早发型子痫前期患者合并HELLP综合征的临床特点,提高及早诊疗能力。方法 回顾性收集2014年3月–2021年10月于浙江大学医学院附属妇产科医院就诊的70例早发型子痫前期合并HELLP综合征(HELLP组)及年龄匹配的140例未合并HELLP综合征早发型子痫前期(对照组)患者一般临床资料、发病特点及实验室检查结果,分析比较两组围产结局。结果 ①两组患者的孕次、产前体质量指数、距前次分娩年限及糖尿病/高血压家族史差异无统计学意义;②与对照组相比,HELLP组孕期最高收缩压、最高舒张压及分娩后住院天数均高于对照组(P<0.001);HELLP组诊断为子痫前期的孕周及分娩孕周早于对照组(P<0.001),且血压升高至分娩的孕周差(P<0.001)、确诊早发型子痫前期至分娩的孕周差均低于对照组(P=0.027);HELLP组子痫发作及胸、腹水的发生率多于对照组(P<0.05)。③HELLP组新生儿入住NICU、发生青紫/苍白窒息的概率更高(P<0.001)。④HELLP组终止妊娠前的谷丙转氨酶、谷草转氨酶、总胆红素、肌酐、尿素、随机葡萄糖、乳酸脱氢酶、活化部分凝血活酶时间及最后一次24 h尿蛋白定量高于对照组(P均<0. 05);血小板低于对照组(P<0. 001)。⑤孕中期血小板计数与HELLP综合征的发生具有显著的相关性(P=0.006),ROC曲线下面积为0.746(95%CI: 0.596~0.897)。结论 早发型子痫前期合并HELLP综合征者较非HELLP综合征者确诊子痫前期的孕周更早,且具有更高的血压、更易发生严重并发症,产后住院时间更长以及新生儿结局亦较差。密切监测早发型子痫前期患者的孕中期血小板计数情况有助于后续HELLP综合征的预测。Abstract:Objective To explore the clinical characteristics of early-onset preeclampsia (PE) combined with HELLP (hemolysis, elevated liver enzymes, and low platelets) syndrome, and to improve the capacity for early diagnosis and treatment.Methods Pregnant women who received treatment at Women’s Hospital, School of Medicine, Zhejiang University between March 2014 and October 2021 were retrospectively enrolled. There were two patient groups, the HELLP group consisting of 70 cases of early-onset PE combined with HELLP syndrome and the control group consisting of 140 cases of early-onset PE without HELLP syndrome. Patients in the two groups were matched by age. The general clinical data, characteristics of pathogenesis, and laboratory findings of the patients were collected and the perinatal outcomes of the two groups were compared and analyzed.Results 1) There was no significant difference in gravidity, pre-delivery body mass index, years from the last delivery, and family history of diabetes mellitus and hypertension between the two groups. 2) The highest systolic blood pressure, highest diastolic blood pressure during the pregnancy, and the postpartum hospital length-of-stay (P<0.001) in the HELLP group were higher than those in the control group. The gestational age at the time of the diagnosis of PE (P=0.001) and the gestational age at delivery (P<0.001) in the HELLP group were significantly earlier than those in the control group. The difference between the gestational age at the time of blood pressure elevation and that at the time of delivery (P<0.001), and the gestational age difference between the diagnosis of early-onset PE and delivery (P=0.027) were lower than those in the control group. The incidences of eclampsia in the HELLP group, pleural effusion, and ascites were higher than those of the control group. 3) Neonates in the HELLP group had a higher probability of being admitted to NICU and developing cyanotic/pale asphyxia (P<0.001). 4) Before the termination of pregnancy, the HELLP group had higher levels of alanine aminotransferase, aspartate aminotransferase, total bilirubin, creatinine, urea, random glucose, lactate dehydrogenase, activated partial thromboplastin time, and the last 24-hour urine protein quantification than those of the control group (all P<0.05), while the platelet (PLT) counts were significantly lower than those of the control group (P<0.001). 5) There was a significant correlation between PLT counts in the second trimester and the onset of HELLP syndrome (P=0.006), with the area under the ROC curve reaching 0.746 (95% CI: 0.596-0.897).Conclusion In comparison with early-onset PE patients without HELLP syndrome, patients with early-onset PE combined with HELLP syndrome are diagnosed for PE at an earlier gestational age, have higher blood pressure, are more prone to serious pregnancy complications, and have longer postpartum hospital length-of-stay and worse neonatal outcomes. Close monitoring of PLT counts of early-onset PE patients in the second trimester may help predict subsequent HELLP syndrome.
-
Keywords:
- HELLP syndrome /
- Early-onset /
- Preeclampsia /
- Retrospective analysis
-
早发型子痫前期是指发生于妊娠34周以前的重度子痫前期[1]。溶血肝功能异常血小板减少综合征(HELLP综合征)是重度子痫前期患者的严重并发症之一,以溶血、肝酶升高以及血小板减少为主要表现[2]。既往已有分别针对早发型子痫前期和HELLP综合征的多方面研究,但对于早发型子痫前期合并HELLP综合征者的临床研究文献较少[3]。因此,本研究对2014年以来在我院就诊并分娩的早发型子痫前期合并HELLP综合征患者进行了回顾性的研究,旨在探讨早发型子痫前期发生HELLP综合征的临床特征,并试图寻找可以预测早发型子痫前期患者进一步发生HELLP综合征的指标。
1. 对象与方法
1.1 对象
回顾性收集2014年3月–2021年10月于浙江大学医学院附属妇产科医院就诊并分娩的70例早发型子痫前期合并HELLP综合征患者(HELLP组)的临床资料,早发型子痫前期合并HELLP综合征的诊断标准采用美国Tennessee诊断标准[3]。对照组则以年龄1∶2匹配的方式随机抽取140例同期于我院产检并分娩的早发型子痫前期未合并HELLP综合征患者。排除标准:①合并肝内胆汁淤积症者;②妊娠合并严重肝肾疾病患者;③妊娠合并血液系统疾病、自身免疫疾病患者;④病例资料不全者。本研究已通过我院道德伦理委员会的审批同意,伦理批准号IRB-20220114-R。
1.2 观察指标
观察两组患者在一般临床资料、母儿情况、孕中期及终止妊娠前实验室结果的差异。①一般临床资料:身高、孕次、产次、距前次分娩的年限、糖尿病与高血压的一级家族史、孕前身体质量指数(body mass index, BMI)等;②此次妊娠情况:最高血压的收缩压与舒张压、住院天数、血压开始升高的孕周、确诊早发型子痫前期的孕周、分娩孕周、剖宫产率、是否辅助生殖、是否子痫发作、产后出血、胸腹水等情况;③新生儿结局:新生儿产后去向〔母婴同室、新生儿科(非重症)、新生儿重症监护室(NICU)〕,新生儿是否青紫窒息(出生后5 min APGAR评分4~7分)/苍白窒息(出生后5 min APGAR评分0~3分);④实验室结果:孕中期及终止妊娠前血常规,凝血功能,乳酸脱氢酶,肝功能(谷丙转氨酶、谷草转氨酶、总胆红素),肾功能(肌酐、尿素),终止妊娠前最后一次24 h尿蛋白定量等。
1.3 统计学方法
计量资料正态分布时以
$ \bar x \pm s $ 表示,组间采用独立样本t检验进行分析,非正态分布时以中位数(P25~ P75)表示,采用非参数检验Mann-Whitney U检验进行分析。计数资料以例数(%)表示,两组间数据采用χ2检验。P<0.05为差异有统计学意义。采用logistic回归分析血小板、谷草转氨酶/血小板与HELLP综合征发生的相关性。相关性的预测效果将通过ROC曲线下的面积(AUC)来表示。
2. 结果
2.1 一般临床资料结果
HELLP组与对照组的孕次(P=0.574)、产次(P=0.521)、距前次分娩年限(P=0.916)、孕前BMI(P=0.796)、糖尿病的一级家族史(P=0.587)、高血压的一级家族史(P=0.632)差异均无统计学意义。
HELLP组与对照组剖宫产率(P=0.359)、辅助生殖(P=0.336)、产后出血(P=0.799)、弥散性血管内凝血(DIC)的发病率(P=0.156)比较均未见明显差异;两组间合并多胎妊娠(P=0.057)、妊娠期糖尿病(P=0.116)、慢性高血压(P=0.497)情况亦无明显差异。HELLP组孕期最高收缩压(P=0.003)、最高舒张压(P<0.001)、住院总天数(P<0.001)及分娩后住院天数(P<0.001)均高于对照组;尽管两组间血压升高的孕周(P=0.156)无明显差异,但HELLP组诊断孕周(P=0.001)及分娩孕周(P<0.001)却明显早于对照组,且血压升高至分娩的孕周差(P<0.001)、确诊孕周至分娩的孕周差(P=0.027)均低于对照组。值得注意的是,HELLP组有2例子痫发作,而对照组则无子痫发作的情况(P=0.044);并且两组胸、腹水发生率差异也有统计学意义(P=0.021)。见表1。
表 1 HELLP组与对照组患者一般临床资料及此次妊娠情况结果Table 1. The general clinical data and the outcomes of the pregnancy under study of the HELLP group and the control groupItem HELLP group
(n=70)Control group
(n=140)Statistic P Chronic hypertension/case (%) 8 (11.4) 21 (15) χ2=0.500 0.479 Multiple gestation/case (%) 6 (8.6) 26 (18.6) χ2=3.613 0.057 Gestational diabetes mellitus/case (%) 10 (14.3) 36 (25.7) χ2=3.563 0.059 Eclampsia attack/case (%) 2 (2.9) 0 (0.0) χ2=4.038 0.044 Postpartum hemorrhage/case (%) 3 (4.3) 6 (4.3) χ2=0.000 1.000 DIC/case (%) 1 (1.4) 0 (0.0) χ2=2.010 0.156 Hydrothorax and ascite/case (%) 13 (18.6) 11 (7.9) χ2=5.292 0.021 Assisted reproduction/case (%) 8 (11.4) 23 (18.6) χ2=0.927 0.336 Caesarean section/case (%) 68 (97.1) 132 (94.3) χ2=0.840 0.359 SBPmax/mmHg 171.20±17.31 163.42±17.34 t=−3.059 0.003 DBPmax/mmHg* 107 (100-115) 100 (94-108.25) z=−3.873 0.000 Length of hospital stay/d 8.97±3.44 11.86±6.76 z=−3.591 0.000 Length of hospital stay after delivery/d* 7 (6-7) 5 (5-6) z=−4.899 0.000 Delivery gestational age/week* 30 (28-32) 33 (31-34) z=−5.386 0.000 Gestational age at the onset of blood pressure elevation/week* 28 (25-30) 29 (24-32) z=−1.420 0.156 Gestational age at diagnosis of PE/week* 29 (27-32) 31 (29-33) z=−3.246 0.001 Gestational age difference between the onset of blood pressure elevation and delivery/week* 2 (0-6) 3 (1-9) z=−3.771 0.000 Gestational age difference between diagnosis of PE and delivery/week* 0 (0-1) 1 (0-2) z=−2.213 0.027 DIC: Disseminated intravascular coagulation; SBPmax: The highest systolic blood pressure; DBPmax: Maximum diastolic blood pressure. * Median (P25-P75). 1 mmHg=0.133 kPa. 2.2 新生儿结局
结果见表2。HELLP组共76例新生儿,其中72例活产新生儿转入NICU(65/72,90.3%)或新生儿科(7/72,9.7%)救治,4例死亡围生儿中2例为人工引产。对照组共有166例新生儿,158例活产新生儿有133例转入NICU(102/158,64.6%)或新生儿科(31/158,19.6%)救治,8例死亡围生儿中7例为人工引产。两组间新生儿去向差异有统计学意义(P<0.001)。HELLP组活产新生儿中出现20.8%(15/72)的新生儿青紫窒息,5.6%(4/72)苍白窒息,而对照组仅发生了5.7%(9/158)新生儿青紫窒息,无苍白窒息(P<0.001)。
表 2 HELLP组与对照组活产新生儿结局Table 2. The outcomes of live births of the HELLP group and the control groupItem HELLP group (n=72) Control group (n=158) z P Status of live births/case (%) 22.050 0.00 Normal 53 (73.6) 149 (94.3) Blue asphyxia 15 (20.8) 9 (5.7) Asphyxia pallida 4 (5.6) 0 (0.0) Where the live-birth newborns went/case (%) 18.832 0.00 Rooming-in 0 (0.0) 25 (15.8) Neonatology department 7 (9.7) 31 (19.6) NICU 65 (90.3) 102 (64.6) 2.3 实验室数据
HELLP组终止妊娠前的谷丙转氨酶、谷草转氨酶、总胆红素、肌酐、尿素、随机葡萄糖、乳酸脱氢酶、活化部分凝血活酶时间、终止妊娠前最后一次24 h尿蛋白定量均高于对照组(P均<0.05),同时血小板低于对照组(P均<0.001)。两组间的其他凝血指标和血脂指标,差异均无统计学意义(P>0.05)。此外,我们还分析了14例HELLP组和54例对照组在24~28孕周血常规及肝功能化验结果,发现两组血小板计数(P=0.003)和谷草转氨酶/血小板比值(P=0.007)差异有统计学意义,但是谷丙转氨酶/血小板比值差异并无统计学意义(P=0.051)。见表3。
表 3 HELLP组与对照组患者实验室结果Table 3. The laboratory findings of the HELLP group and the control groupItem HELLP group (n=70) Control group (n=140) Statisic P Second trimester* Blood platelet/(×109 L-1) 183.86±51.25 231.07±50.50 t=3.108 0.003 ALT/(U/L) 17.36 (12.25-25.25) 16.52 (10.75-19.25) z=−0.729 0.466 AST/(U/L) 19.21 (15.00-23.25) 18.17 (13.00-20.00) z=−1.209 0.227 TB/(μmol/L) 6.85 (5.23-8.85) 5.7 (4.3-7.1) z=−1.566 0.117 ALT/PLT 0.09 (0.06-0.15) 0.06 (0.04-0.09) z=−1.953 0.051 AST/PLT 0.11 (0.06-0.18) 0.08 (0.03-0.33) z=−2.677 0.007 Antepartum Blood platelet/(×109 L-1) 95.51±40.85 182.14±53.89 t=11.849 0.000 APTT/s 35.38±3.84 32.51±2.99 t=−5.930 0.000 Fibrinogen/(g/L) 3.83±1.12 4.08±1.02 t=1.635 0.104 Prothrombin time/s 12.30 (11.80-12.73) 12.10 (11.70-12.50) z=−1.794 0.073 LDL/(mmol/L) 3.11 (2.44-4.04) 3.19 (2.68-4.03) z=−0.775 0.438 HDL/(mmol/L) 1.62 (1.43-2.13) 1.59 (1.38-1.83) z=−1.399 0.162 Total cholesterol/(mmol/L) 6.40±1.40 6.29±1.37 t=−0.43 0.668 Triglyceride/(mmol/L) 3.20 (2.36-3.99) 3.62 (2.72-4.40) z=−1.943 0.052 ALT/(U/L) 63.00 (23.50-142.50) 16.00 (10.00-22.00) z=−8.047 0.000 AST/(U/L) 55.00 (33.00-106.75) 20.00 (15.00-27.00) z=−9.119 0.000 TB/(μmol/L) 9.45 (5.80-15.55) 5.50 (4.33-7.48) z=−6.092 0.000 Creatinine/(μmol/L) 73.95 (62.63-86.88) 59.45 (51.00-69.00) z=−5.416 0.000 Urea/(mmol/L) 5.55 (4.30-8.07) 4.48 (3.63-5.68) z=−3.622 0.000 Random glucose/(mmol/L) 6.19 (4.81-7.38) 4.93 (4.18-5.68) z=−4.298 0.000 Lactic dehydrogenase/(U/L) 271.00 (215.00-409.00) 199.00 (176.00-232.00) z=−5.023 0.000 24 h urine protein/g 6.08 (1.92-8.26) 2.37 (0.378-5.66) z=−2.638 0.008 * HELLP group n=14, control group n=54; ALT: Alanine aminotransferase; PLT: Platelets; AST: Glutamic oxalacetic transaminase; GPT: Glutamic-pyruvic transaminase; TB: Total bilirubin; APTT: Activated partial thromboplastin time; LDL: Low density lipoprotein; HDL: High density lipoprotein. 2.4 孕中期血小板及谷草转氨酶/血小板比值与HELLP综合征的发生相关性分析
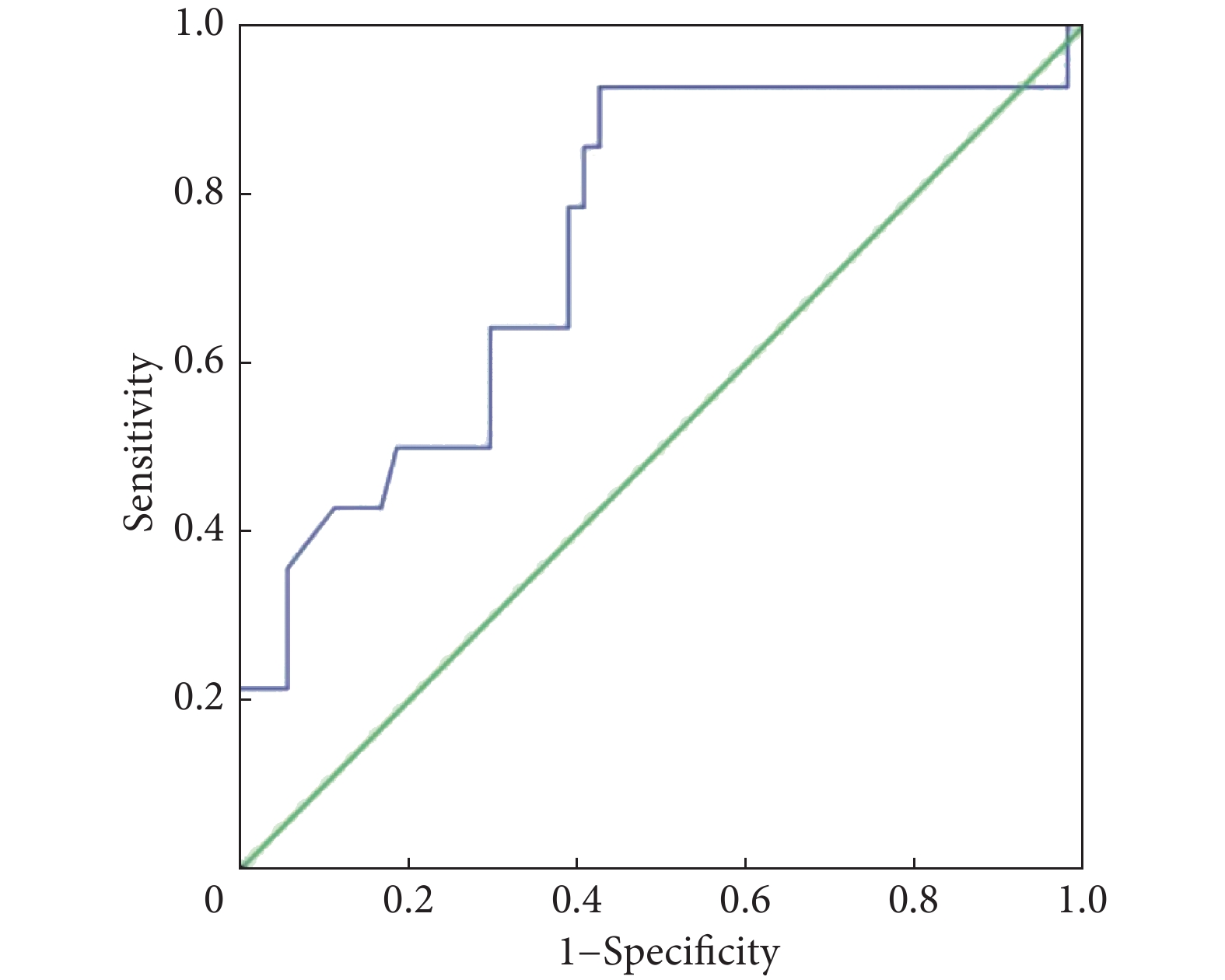
由于发现HELLP组与对照组在孕中期的血小板计数及谷草转氨酶/血小板比值有明显的差异,故将两项指标与HELLP是否发生分别进行logistic回归单因素分析后得出(表4),孕中期血小板计数与早发型子痫前期患者中HELLP综合征具有显著的相关性,而孕中期谷草转氨酶/血小板比值则未体现与HELLP综合征的相关性,ROC曲线直观说明了孕中期血小板计数对于HELLP综合征的预测效果,曲线下面积为0.746(95%CI: 0.596~0.897),见图1。
表 4 孕中期HELLP 综合征患者的logistic 回归分析Table 4. The logistic regression of HELLP syndrome patients in the second trimesterVariable B SE Wald P OR 95% CI PLT −0.021 0.007 7.592 0.006 0.98 0.965-0.994 AST/PLT 11.584 6.489 3.186 0.074 107357.76 0.321-35864346438.7 PLT: Platelets; AST: Glutamic oxalacetic transaminase; β: Partial regression coefficient; SE: Standard error; OR: Odds ratio; CI: Confidence interval. 3. 讨论
3.1 早发型子痫前期合并HELLP综合征的高危因素
本研究发现早发型子痫前期合并HELLP综合征与对照组在妊娠经过、实验室数据和围产结局存在明显差异,尤其发现孕中期血小板计数可以帮助尽早识别HELLP综合征。而两组人口学特征差异无显著性。既往多个研究报道HELLP综合征相关的危险因素,但结果不一致。徐宝兰等[4]发现年龄≥35 岁、BMI≥28 kg/m2、孕次≥5次为并发 HELLP 综合征的独立危险因素。MALMSTRÖM等[5]在一项涉及1999–2014年挪威所有登记的生育妇女队列研究中,发现BMI≥30 kg/m2 和糖尿病与 HELLP 综合征在第1次怀孕时相关,而慢性高血压和多胎妊娠与第1次和第2次妊娠的HELLP综合征有关。吕鑫等[6]亦认为高血压家族史、辅助生殖均是早发型子痫前期高危因素。但本研究发现孕前BMI、孕产次、高血压/糖尿病家族史、多胎妊娠、辅助生殖、妊娠期糖尿病均与HELLP综合征无关联。结果不一致的可能原因是本研究样本量不足,此外,本研究两组对象均为早发型子痫前期患者,一般临床资料区别并不大。因此,仍需进行更大样本的研究,从而验证早发型子痫前期合并HELLP综合征的人口学特征。
本文发现HELLP组孕期血压升高明显,诊断孕周和分娩孕周均早于对照组。且血压升高至分娩的孕周差、确诊早发型子痫前期至分娩的孕周差明显低于对照组。HELLP组住院总天数虽少于对照组,但术后住院时间明显长于对照组。以上结果意味着HELLP组患者发病更早、发展迅速、病情更重。王媛等[7]在一项队列研究中发现不同孕期收缩压、舒张压每增加1 mmHg,子痫前期发生风险增加至47%(早孕期),晚孕期进一步升高,预产期者该风险达100%。同时建议对于早中孕期血压≥120 mmHg或舒张压≥90 mmHg的妇女,有必要加强血压监测,增加产检频率等方式,尽早识别子痫前期发生。
3.2 早发型子痫前期合并HELLP综合征的母儿结局
本研究中HELLP组有2例子痫发作(2.9%)和1例DIC(1.4%),同时HELLP组胸腹水发生率(18.6%)亦高于对照组(7.9%),但产后出血、剖宫产率两组无明显差异。曾有报道HELLP综合征不仅是子痫前期的严重并发症之一,也是子痫发作的一个高危因素[8]。DURUGKAR等[9]发现HELLP综合征最常见的母体并发症为DIC (14.1%)和子痫发作(21.1%),其基本病理生理改变包括血管内皮细胞激活和血小板下降、溶血,极易导致DIC。另外,HELLP组新生儿进入NICU救治和窒息率以及死胎率高(P<0.001)。既往研究亦表明,新生儿不良结局多数与早产后胎儿不成熟、低出生体质量有关[9],因此我们推测HELLP组是由于病情严重而提前分娩导致。
3.3 早发型子痫前期合并HELLP综合征检验指标预测价值
HELLP组终止妊娠前的24 h尿蛋白定量(P=0.008)明显高于对照组,终止妊娠前肝肾功能、总胆红素、随机葡萄糖、乳酸脱氢酶、活化部分凝血活酶时间结果均高于对照组。KANG等[10]对210名HELLP综合征患者,210名单纯子痫前期患者及210名健康孕妇纳入研究,发现三组血小板比较差异有统计学意义(P均=0.000),从低到高分别为HELLP组(43.4×109 L-1)、对照组(180.5×109 L-1)和子痫前期组(181.5×109 L-1),提示血小板计数是区别HELLP综合征与子痫前期的重要指标。GEDIK等[11]对77名HELLP综合征分析后发现血小板计数低、延长的活化凝血活酶时间、高总胆红素、高乳酸脱氢酶、高血尿素氮和肌酐,而且这些指标均与HELLP综合征相关不良并发症及死亡率的高风险相关,与本研究结果相似。
由于HELLP综合征缺乏特异性的症状和体征,从检验结果分析亦不是所有的患者均表现出血小板降低或肝功能升高的情况[12],因此如何提前预测HELLP综合征的发生成为了一项重要的命题。本研究通过logistic回归发现孕中期血小板计数与HELLP综合征的发生显著相关(P=0.006),并且ROC曲线下面积达0.746,提示孕中期血小板计数对早发型子痫前期患者中预测HELLP综合征的发生具有一定的效果。TOLUNAY等[13]对42例HELLP综合征及74例正常对照孕妇研究后发现孕早期谷草转氨酶/血小板值对发生HELLP综合征具有预测价值。本研究则尝试使用谷丙转氨酶/血小板比值或谷草转氨酶/血小板比值指标预测HELLP综合征,但遗憾的是我们并未获取到孕早期数据,同时孕中期数据虽提示谷草转氨酶/血小板比值在HELLP组与对照组之间差异有统计学意义,但logistic回归中未提示显著相关性,这可能与样本量过少有关。后续的研究可考虑获取更多的孕早期、孕中期化验结果,增加更多的预测指标,提高预测HELLP综合征患者的效率以便早日识别风险,提前进行孕期管理和干预。
总之,早发型子痫前期合并HELLP综合征与不合并HELLP综合征者在人口学指标方面无明显差异。但合并HELLP综合征者更易发生子痫、胸腹水等并发症,活产新生儿转入ICU及发生窒息的概率升高。两组存在明显的检验结果差异,孕中期血小板计数有助于HELLP综合征的预测。早发型子痫前期患者如有孕中期血小板偏低者应警惕后续HELLP综合征的发生,及时诊治以减少母儿不良结局的发生。但是本研究为单中心的回顾性研究,对居住在浙江省杭州市及周边地区的患者代表性较好,但仍需全国范围内多中心更大样本量的研究以获得更多病例资料。同时,本研究选择了早发型子痫前期患者中合并HELLP综合征与未合并HELLP综合征患者进行了研究对比,没有设置正常妊娠作为对照组,下一步可考虑纳入正常妊娠患者,进一步扩大研究范围。同时还应收录更多孕中期化验信息,以期更早识别早发型子痫前期及HELLP综合征的高危因素,更好预测并预防它们的发生。
* * *
利益冲突 所有作者均声明不存在利益冲突
-
表 1 HELLP组与对照组患者一般临床资料及此次妊娠情况结果
Table 1 The general clinical data and the outcomes of the pregnancy under study of the HELLP group and the control group
Item HELLP group
(n=70)Control group
(n=140)Statistic P Chronic hypertension/case (%) 8 (11.4) 21 (15) χ2=0.500 0.479 Multiple gestation/case (%) 6 (8.6) 26 (18.6) χ2=3.613 0.057 Gestational diabetes mellitus/case (%) 10 (14.3) 36 (25.7) χ2=3.563 0.059 Eclampsia attack/case (%) 2 (2.9) 0 (0.0) χ2=4.038 0.044 Postpartum hemorrhage/case (%) 3 (4.3) 6 (4.3) χ2=0.000 1.000 DIC/case (%) 1 (1.4) 0 (0.0) χ2=2.010 0.156 Hydrothorax and ascite/case (%) 13 (18.6) 11 (7.9) χ2=5.292 0.021 Assisted reproduction/case (%) 8 (11.4) 23 (18.6) χ2=0.927 0.336 Caesarean section/case (%) 68 (97.1) 132 (94.3) χ2=0.840 0.359 SBPmax/mmHg 171.20±17.31 163.42±17.34 t=−3.059 0.003 DBPmax/mmHg* 107 (100-115) 100 (94-108.25) z=−3.873 0.000 Length of hospital stay/d 8.97±3.44 11.86±6.76 z=−3.591 0.000 Length of hospital stay after delivery/d* 7 (6-7) 5 (5-6) z=−4.899 0.000 Delivery gestational age/week* 30 (28-32) 33 (31-34) z=−5.386 0.000 Gestational age at the onset of blood pressure elevation/week* 28 (25-30) 29 (24-32) z=−1.420 0.156 Gestational age at diagnosis of PE/week* 29 (27-32) 31 (29-33) z=−3.246 0.001 Gestational age difference between the onset of blood pressure elevation and delivery/week* 2 (0-6) 3 (1-9) z=−3.771 0.000 Gestational age difference between diagnosis of PE and delivery/week* 0 (0-1) 1 (0-2) z=−2.213 0.027 DIC: Disseminated intravascular coagulation; SBPmax: The highest systolic blood pressure; DBPmax: Maximum diastolic blood pressure. * Median (P25-P75). 1 mmHg=0.133 kPa. 表 2 HELLP组与对照组活产新生儿结局
Table 2 The outcomes of live births of the HELLP group and the control group
Item HELLP group (n=72) Control group (n=158) z P Status of live births/case (%) 22.050 0.00 Normal 53 (73.6) 149 (94.3) Blue asphyxia 15 (20.8) 9 (5.7) Asphyxia pallida 4 (5.6) 0 (0.0) Where the live-birth newborns went/case (%) 18.832 0.00 Rooming-in 0 (0.0) 25 (15.8) Neonatology department 7 (9.7) 31 (19.6) NICU 65 (90.3) 102 (64.6) 表 3 HELLP组与对照组患者实验室结果
Table 3 The laboratory findings of the HELLP group and the control group
Item HELLP group (n=70) Control group (n=140) Statisic P Second trimester* Blood platelet/(×109 L-1) 183.86±51.25 231.07±50.50 t=3.108 0.003 ALT/(U/L) 17.36 (12.25-25.25) 16.52 (10.75-19.25) z=−0.729 0.466 AST/(U/L) 19.21 (15.00-23.25) 18.17 (13.00-20.00) z=−1.209 0.227 TB/(μmol/L) 6.85 (5.23-8.85) 5.7 (4.3-7.1) z=−1.566 0.117 ALT/PLT 0.09 (0.06-0.15) 0.06 (0.04-0.09) z=−1.953 0.051 AST/PLT 0.11 (0.06-0.18) 0.08 (0.03-0.33) z=−2.677 0.007 Antepartum Blood platelet/(×109 L-1) 95.51±40.85 182.14±53.89 t=11.849 0.000 APTT/s 35.38±3.84 32.51±2.99 t=−5.930 0.000 Fibrinogen/(g/L) 3.83±1.12 4.08±1.02 t=1.635 0.104 Prothrombin time/s 12.30 (11.80-12.73) 12.10 (11.70-12.50) z=−1.794 0.073 LDL/(mmol/L) 3.11 (2.44-4.04) 3.19 (2.68-4.03) z=−0.775 0.438 HDL/(mmol/L) 1.62 (1.43-2.13) 1.59 (1.38-1.83) z=−1.399 0.162 Total cholesterol/(mmol/L) 6.40±1.40 6.29±1.37 t=−0.43 0.668 Triglyceride/(mmol/L) 3.20 (2.36-3.99) 3.62 (2.72-4.40) z=−1.943 0.052 ALT/(U/L) 63.00 (23.50-142.50) 16.00 (10.00-22.00) z=−8.047 0.000 AST/(U/L) 55.00 (33.00-106.75) 20.00 (15.00-27.00) z=−9.119 0.000 TB/(μmol/L) 9.45 (5.80-15.55) 5.50 (4.33-7.48) z=−6.092 0.000 Creatinine/(μmol/L) 73.95 (62.63-86.88) 59.45 (51.00-69.00) z=−5.416 0.000 Urea/(mmol/L) 5.55 (4.30-8.07) 4.48 (3.63-5.68) z=−3.622 0.000 Random glucose/(mmol/L) 6.19 (4.81-7.38) 4.93 (4.18-5.68) z=−4.298 0.000 Lactic dehydrogenase/(U/L) 271.00 (215.00-409.00) 199.00 (176.00-232.00) z=−5.023 0.000 24 h urine protein/g 6.08 (1.92-8.26) 2.37 (0.378-5.66) z=−2.638 0.008 * HELLP group n=14, control group n=54; ALT: Alanine aminotransferase; PLT: Platelets; AST: Glutamic oxalacetic transaminase; GPT: Glutamic-pyruvic transaminase; TB: Total bilirubin; APTT: Activated partial thromboplastin time; LDL: Low density lipoprotein; HDL: High density lipoprotein. 表 4 孕中期HELLP 综合征患者的logistic 回归分析
Table 4 The logistic regression of HELLP syndrome patients in the second trimester
Variable B SE Wald P OR 95% CI PLT −0.021 0.007 7.592 0.006 0.98 0.965-0.994 AST/PLT 11.584 6.489 3.186 0.074 107357.76 0.321-35864346438.7 PLT: Platelets; AST: Glutamic oxalacetic transaminase; β: Partial regression coefficient; SE: Standard error; OR: Odds ratio; CI: Confidence interval. -
[1] POON L C, SHENNAN A, HYETT J A, et al. The International Federation of Gynecology and Obstetrics (FIGO) initiative on pre-eclampsia: A pragmatic guide for first-trimester screening and prevention: A pragmatic guide for first-trimester screening and prevention. Int J Gynaecol Obstet,2019,145(S1): 1–33. DOI: 10.1002/ijgo.12802
[2] SIBAI B M. Diagnosis, controversies, and management of the syndrome of hemolysis, elevated liver enzymes, and low platelet count. Obstet Gynecol,2004,103(5): 981–991. DOI: 10.1097/01.AOG.0000126245.35811.2a
[3] KINAY T, KÜÇÜK C, KAYIKÇIOĞLU F, et al. Severe preeclampsia versus HELLP syndrome: Maternal and perinatal outcomes at <34 and ≥34 weeks’ gestation. Balkan Med J,2015,32(4): 359–363. DOI: 10.5152/balkanmedj.2015.15777
[4] 徐宝兰, 辛崇敏, 卢培玲. 妊娠期高血压疾病孕妇的妊娠结局及其并发hellp综合征的影响因素. 广西医学,2021,43(3): 6–9. [5] MALMSTRÖM O, MORKEN N H. HELLP syndrome, risk factors in first and second pregnancy: a population-based cohort study. Acta Obstet Gynecol Scand,2018,97(6): 709–716. DOI: 10.1111/aogs.13322
[6] 吕鑫, 张为远, 张靖霄, 等. 早发与晚发子痫前期高危因素的对比分析. 中华妇产科杂志,2021,56(11): 760–766. DOI: 10.3760/cma.j.cn112141-20210330-00164 [7] 王媛, 唐慧荣, 王娅, 等. 孕期血压与妊娠期高血压或子痫前期发病关系的研究. 中华妇产科杂志,2021,56(11): 767–773. DOI: 10.3760/cma.j.cn112141-20210601-00297 [8] ALESE M O, MOODLEY J, NAICKER T. Preeclampsia and HELLP syndrome, the role of the liver. J Matern Fetal Neonatal Med,2021,34(1): 117–123. DOI: 10.1080/14767058.2019.1572737
[9] DURUGKAR K. A study of maternal and perinatal outcome in cases of HELLP and partial HELLP syndrome. Int J Reprod Contracept Obstet Gynecol,2017,6(12): 5491–5496. DOI: 10.18203/2320-1770.ijrcog20175267
[10] KANG S Y, WANG Y, ZHOU L P, et al. New indicators in evaluation of hemolysis, elevated liver enzymes, and low platelet syndrome: A case-control study. World J Clin Cases,2021,9(6): 1259–1270. DOI: 10.12998/wjcc.v9.i6.1259
[11] GEDIK E, YÜCEL N, SAHIN T, et al. Hemolysis, elevated liver enzymes, and low platelet syndrome: Outcomes for patients admitted to intensive care at a tertiary referral hospital. Hypertens Pregnancy,2017,36(1): 21–29. DOI: 10.1080/10641955.2016.1218505
[12] WALLACE K, HARRIS S, ADDISON A, et al. HELLP Syndrome: Pathophysiology and Current Therapies. Curr Pharm Biotechnol,2018,19(10): 816–826. DOI: 10.2174/1389201019666180712115215
[13] TOLUNAY H E, KAHRAMAN N C, VARLI E N, et al. Can first-trimester AST to platelet ratio index scores predict HELLP syndrome? J Coll Physicians Surg Pak,2021,31(2): 188–192. DOI: 10.29271/JCPSP.2021.02.188
-
期刊类型引用(1)
1. 吴亚男,郝媛媛,安泓润. miR-224、ATG5在早发型子痫前期中的预测价值. 检验医学与临床. 2025(07): 974-977 .  百度学术
百度学术
其他类型引用(0)

 首页
首页



 下载:
下载: