Preliminary Study of Dilated Cardiomyopathy at a High Altitude Based on Cardiac Magnetic Resonance Feature Tracking
-
摘要:目的
探讨心脏磁共振特征追踪(cardiovascular magnetic resonance feature tracking, CMR-FT)技术在高海拔地区扩张型心肌病(dilated cardiomyopathy, DCM)患者心肌应变中的初步应用。
方法回顾性搜集高海拔DCM患者(patients with DCM at high altitude, DCM-H)、平原DCM患者(patients with DCM at plain, DCM-P)、高海拔健康志愿者(healthy volunteers at high altitude, HV-H)、平原健康志愿者(healthy volunteers at high altitude, HV-P)各29例、27例、23例、24例。所有受试者均进行了3.0T MRI快速平衡稳态自由进动电影序列扫描。所获得的CMR图像使用cvi42后处理软件进行分析,获得左室心功能参数及心肌应变参数。
结果DCM-H组左室舒张末容积和收缩末容积高于HV-H组,射血分数、每搏输出量低于HV-H组(所有P<0.01)。DCM-H组与DCM-P组心功能差异无统计学意义。与HV-H相比,DCM-H组整体径向、周向、纵向应变(%)(14.5±6.5 vs. 34.2±10.7; -11.1±4.4 vs. -19.9±2.8; -7.7±3.2 vs. -13.6±4.1)绝对值更低,差异有统计学意义(所有P<0.001)。DCM-H组比DCM-P组整体径向、周向、纵向应变绝对值(%)高(14.5±6.5 vs. 7.0±2.7; -11.1±4.4 vs. -5.4±2.2; -7.7±3.2 vs. -4.3±1.7; 所有P<0.01)。
结论高海拔DCM患者的心肌应变低于高海拔健康志愿者,高于平原DCM患者。CMR-FT可以定量评估高海拔地区DCM患者心肌收缩能力,在临床应用中具有较好的前景。
Abstract:ObjectiveTo investigate the application of cardiovascular magnetic resonance feature tracking (CMR-FT) in assessing myocardial strain in dilated cardiomyopathy (DCM) patients residing at high altitudes.
MethodsWe retrospectively enrolled 29 DCM patients living at high altitudes (DCM-H), 27 DCM patients living in a low-altitude plain environment (DCM-P), 23 healthy volunteers living at a high altitude (HV-H), and 24 healthy volunteers living in a low-altitude plain environment (HV-P). All subjects underwent cine MRI scanning using a 3.0T rapid steady-state free precession sequence. The CMR images thus acquired were analyzed using cvi42, a post-processing software, to obtain left ventricular function and myocardial strain parameters.
ResultsCompared with the HV-H group, the DCM-H group showed higher left ventricle end-diastolic volume (LVEDV) and left ventricle end-systolic volume (LVESV), and lower left ventricular ejection fraction (LVEF) and stroke volume ( LVSV) (all P < 0.01). No significant difference was observed in cardiac function between the DCM-H and DCM-P groups (all P > 0.05). The absolute values of global radial strain (GRS), global circumferential strain (GCS), and global longitudinal strain (GLS) in the DCM-H group were lower than those in the HV-P group ([14.5 ± 6.5]% vs. [34.2 ± 10.7]%, [-11.1 ± 4.4]% vs. [-19.9 ± 2.8]%, and [-7.7 ± 3.2]% vs. [-13.6 ± 4.1]%, respectively), with the differences being statistically significant (all P < 0.001). The DCM-H group had higher absolute GRS, GCS, and GCS values than the DCM-P group did ([14.5 ± 6.5]% vs. [7.0 ± 2.7]%, [-11.1 ± 4.4]% vs. [-5.4 ± 2.2]%, and [-7.7 ± 3.2]% vs. [-4.3 ± 1.7]%, respectivley, all P < 0.01).
ConclusionMyocardial strain in DCM patients living at a high altitude is lower than that in healthy volunteers living at a high altitude, but higher than that in DCM patients living in a low-altitude plain environment. CMR-FT can be used to quantitatively assess myocardial contractility in DCM patients living at a high altitude, showing promise for clinical application.
-
Keywords:
- CMR-FT /
- Dilated cardiomyopathy /
- High altitude /
- Myocardial strain
-
扩张型心肌病(dilated cardiomyopathy, DCM)是一种以左心室或双心室扩张伴收缩功能障碍为特征的异质性心肌病,心肌纤维化是该病的常见组织病理学特征;临床表现包括心衰、心律失常、代谢异常、血栓栓塞和猝死[1-2]。心脏磁共振(cardiovascular magnetic resonance, CMR)组织分辨率高,能够通过多参数、多序列成像的方式评估出心脏功能和其组织特征[3-4]。其中,CMR特征追踪(CMR feature tracking, CMR-FT)技术可以评估DCM患者的心肌应变,了解患者心肌收缩功能,并预测患者最终结局[5-6]。高海拔人群长时间面临低氧、低气压、低温为特点的环境,机体通过代偿性低氧调节反应,对心脏结构产生影响[7-11]。目前,CMR-FT对DCM患者心肌应变的研究主要集中在低海拔患者,对于世居高海拔地区或移居高海拔地区人群的研究尚未见报道。本研究旨在通过CMR-FT评估高海拔DCM患者的心肌应变特征,比较高海拔DCM患者与低海拔DCM患者心肌应变特征的差异。
1. 资料与方法
1.1 研究对象
根据世界卫生组织认定标准,海拔高于
2500 m 即为高海拔地区。于本院(海拔约500 m)回顾性搜集2020年6月–2024年3月确诊的高海拔DCM患者(高于2500 m,DCM patients living at a high altitude, DCM-H)、平原DCM患者(海拔约500 m;DCM patients living in low-altitude plain environment, DCM-P)各29例、27例。DCM患者纳入标准:①参考美国心脏协会、美国心脏病协会、欧洲心脏病协会诊断标准,即患者左心室舒张末容积(left ventricle end-diastolic volume, LVEDV)大于正常人2倍标准差,且左心室射血分数(left ventricular ejection fraction, LVEF)<50%[1, 12];②患者进行CMR扫描前未接受DCM相关治疗。排除标准:①伴有缺血性心脏病、其他类型非缺血性心肌病、瓣膜病、先天性心脏病。②图像质量不能满足图像后处理的要求。同时搜集在这期间年龄、性别匹配的高海拔健康志愿者(healthy volunteers lving at a high altitude, HV-H)23例,平原健康志愿者(healthy volunteers living in low-altitude plain environment, HV-P)24例。健康志愿者无心脑血管疾病,且心电图、超声心动图、血压、血常规、胸部CT正常。本研究通过四川大学华西医院伦理委员会批准(2015年审304号)。1.2 检查方法
所有受试者均在3.0T CMR(Magnetom Tim Trio,西门子,德国)进行快速平衡稳态自由进动(steady-state free precession, SSFP)电影序列扫描。检查前准备包括去除金属异物、进行屏气训练。序列参数:重复时间为3.4 ms,回波时间为1.3 ms;翻转角度为50°;视野为300 mm×340 mm;矩阵大小为256×144;层厚为8 mm,层间距为0;带宽为100 kHz。通过扫描获得左心室两腔心(短轴和长轴)、三腔心、四腔心图像。
1.3 图像分析
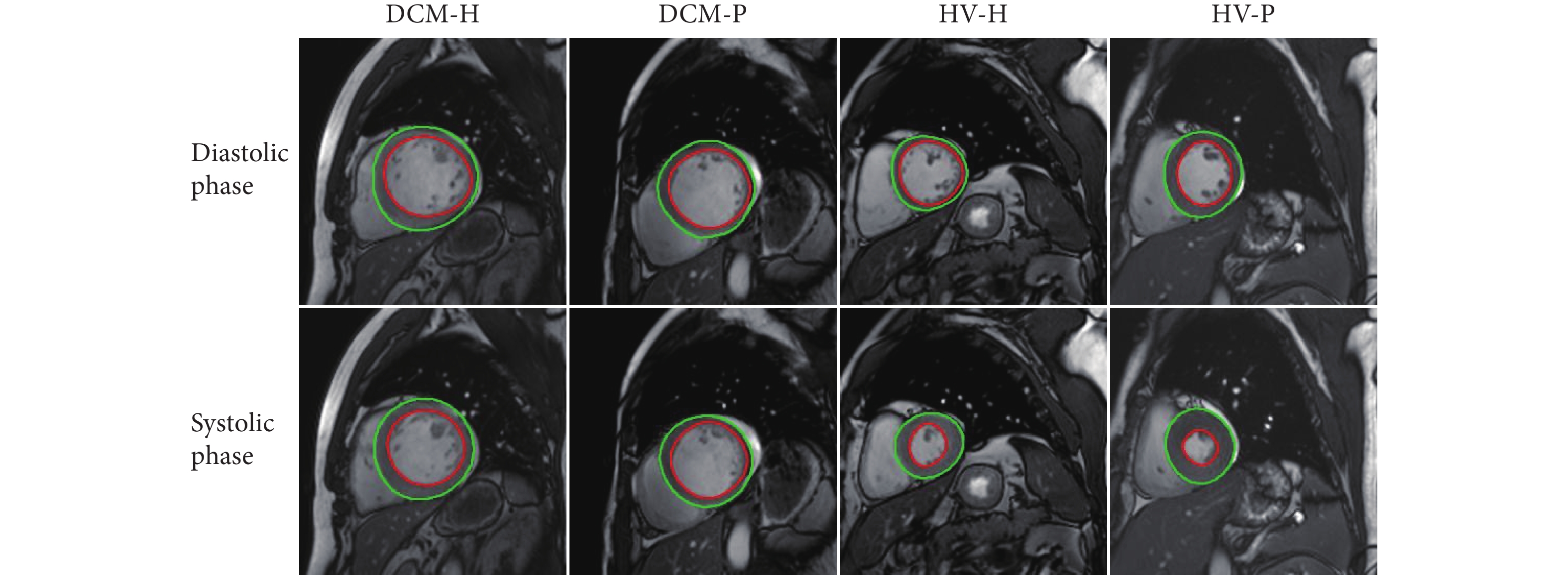
两名具有五年以上经验的心脏影像学医师采用cvi42软件分析心功能及心肌应变。采用自动勾画功能勾勒心内膜及心外膜轮廓(图1),必要时对轮廓进行手动校正,勾画图像包括短轴位、二腔心以及四腔心长轴位。经过软件处理获得心功能及心肌应变参数,包括LVEF、LVEDV、左心室收缩末容积(left ventricle end-systolic volume, LVESD)、左心室每搏输出量(left ventricle stroke volume, LVSV)和左心室整体径向应变(global radial strain, GRS)、周向应变(global circumferential strain, GCS)、纵向应变(global longitudinal strain, GLS)。
![]() 图 1 舒张期与收缩期CMR图像及心内外膜勾画Figure 1. Diastolic and systolic CMR images and outlining of endocardium and epicardiumDCM-H: patient with dilated cardiomyopathy living at a high altitude; DCM-P: patient with dilated cardiomyopathy in low-altitude plain regions; HV-H: healthy volunteer living at a high altitude; HV-P: healthy volunteer in low-altitude plain regions. The green line traces the epicardium, and the red line marks the endocardium.
图 1 舒张期与收缩期CMR图像及心内外膜勾画Figure 1. Diastolic and systolic CMR images and outlining of endocardium and epicardiumDCM-H: patient with dilated cardiomyopathy living at a high altitude; DCM-P: patient with dilated cardiomyopathy in low-altitude plain regions; HV-H: healthy volunteer living at a high altitude; HV-P: healthy volunteer in low-altitude plain regions. The green line traces the epicardium, and the red line marks the endocardium.1.4 统计学方法
所有受试者数据均使用SPSS 22.0软件(IBM Corp,美国)进行统计分析。正态性检验采用Shapiro-Wilk检验。符合正态分布的计量资料以$ \bar{x} \pm s$表示,非正态分布的数据经对数转换呈正态分布后进行分析。方差齐则采用单因素方差分析比较DCM-H、DCM-P、HV-H、HV-P四组数据,若差异有统计学意义,则进一步采用Bonferroni检验进行DCM-H与DCM-P、DCM-H与HV-H、HV-H与HV-P两两比较。方差不齐则采用Welch's ANOVA比较四组差异,差异有统计学意义则通过Games-Howell检验进行两两比较。分类数据分析使用卡方检验。心功能与心肌应变之间的关系采用Pearson相关分析。P<0.05为差异有统计学意义。
2. 结果
2.1 受试者基本资料
所有受试者的基本资料见表1。所有受试者性别、年龄、体质量、身高差异无统计学意义(所有P>0.05)。DCM-H组心率低于DCM-P组(P<0.05)。DCM-H组的收缩压、舒张压、心率比HV-H组低(所有P<0.01)。HV-H组收缩压和舒张压比HV-P组高(P=0.01)。
表 1 受试者基本资料Table 1. Basic data of the subjectsVariable DCM-H (n = 29) DCM-P (n = 27) HV-H (n = 23) HV-P (n = 24) P F Age/yr. 42.2 ± 13.2 44.2 ± 13.2 38.8 ± 10.9 44.3 ± 14.5 0.433 0.921 Male/case (%) 19 (65.5) 17 (63.0) 12 (52.2) 13 (54.2) 0.715 1.359 Body mass/kg 66.8 ± 16.0 66.9 ± 10.3 63.4 ± 15.0 66.6 ± 9.7 0.27 1.344 Height/cm 166.1 ± 7.2 164.6 ± 9.1 166.0 ± 10.7 163.0 ± 8.9 0.589 0.644 SBP/mmHg 112.0 ± 20.9## 111.5 ± 19.4 129.5 ± 6.8^ 115.0 ± 14.9 < 0.001 14.365 DBP/mmHg 72.3 ± 15.6## 74.9 ± 11.8 84.8 ± 5.7^^^ 76.0 ± 9.1 0.001 12.000 HR/min-1 77.7 ± 15.6*, ## 91.5 ± 19.3 91.8 ± 8.6 85.3 ± 9.1 0.001 6.245 SBP: systolic blood pressure; DBP: diastolic blood pressure; HR: heart rate; the other abbreviations are explained in the notes to Fig 1. * P < 0.05, vs. DCM-P; ## P < 0.01, vs. HV-H; ^ P < 0.05, ^^^ P < 0.001, vs. HV-P. The data are expressed as $ \bar{x} \pm s$ except those for sex. 1 mmHg = 0.133 kPa. All the variables are analyzed by Welch's test except for body mass, which is analyzed by one-way ANOVA. 2.2 受试者心功能参数和心肌应变
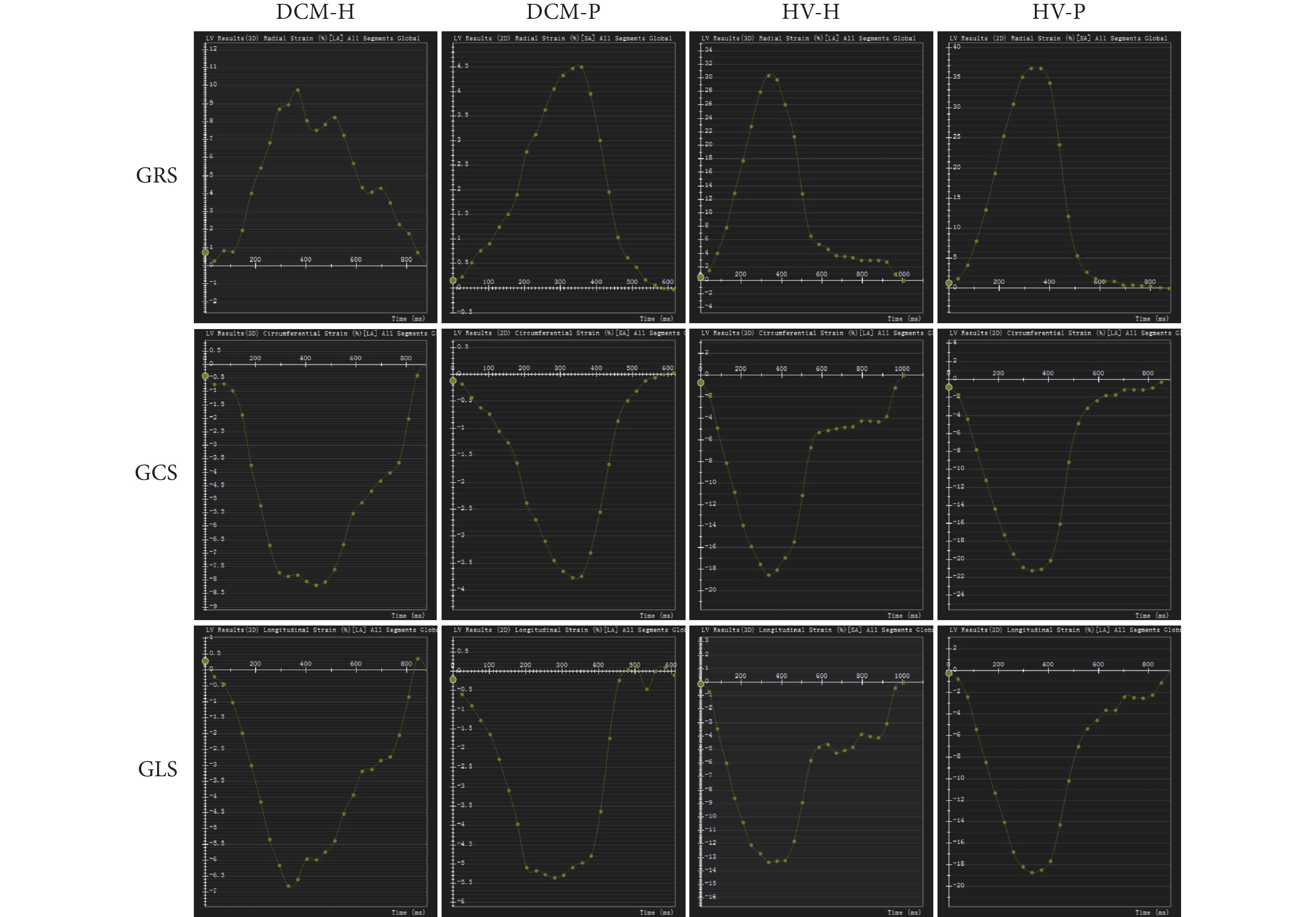
所有受试者的心功能及心肌应变参数见表2、表3。相比于HV-H组,DCM-H组LVEDV和LVESV更高,且LVEF、LVSV更低(所有P<0.01)。DCM-H组与DCM-P组心功能相似(所有P>0.05)。HV-H组对比HV-P组,LVEDV、LVESV、LVSV均更高(所有P<0.001),而LVEF的差异无统计学意义(P>0.05)。DCM-H组对比HV-H组,GRS、GCS、GLS绝对值均更低(所有P<0.001)。DCM-H组比DCM-P组GRS、GCS、GLS绝对值更高(所有P<0.01)。HV-H组GRS、GCS绝对值均比HV-P组低(两者P<0.05)。各组心肌应变代表图见图2。
表 2 受试者心功能参数Table 2. Cardiac function parameters of the subjectsParameter DCM-H (n = 29) DCM-P (n = 27) HV-H (n = 23) HV-P (n = 24) P F LVEF/% 25.5 ± 11.7### 18.4 ± 3.8 61.2 ± 6.0 64.3 ± 5.2 < 0.001 300.8 LVEDV/mL 303.2 ± 96.8### 329.1 ± 43.7 145.6 ± 34^^^ 85.1 ± 20.3 < 0.001 268.7 LVESV/mL 231.6 ± 101.9### 268.9 ± 34.7 59.3 ± 25.7^^^ 32.3 ± 11.4 < 0.001 327.5 LVSV/mL 71.6 ± 18.2## 60.3 ± 21.7 86.3 ± 13.2^^^ 52.8 ± 14.6 < 0.001 26.8 LVEF: left ventricular ejection fraction; LVEDV: left ventricle end-diastolic volume; LVESV: left ventricle end-systolic volume; LVSV: left ventricle stroke volume. The other abbreviations are explained in the notes to Fig 1. ## P < 0.01, ### P < 0.001, vs. HV-H; ^^^ P < 0.001, vs. HV-P. The data are expressed as $ \bar{x} \pm s$. All parameters are analyzed by Welch's test. 表 3 受试者心肌应变参数Table 3. Myocardial strain of parameters the subjectsParameter DCM-H (n = 29) DCM-P (n = 27) HV-H (n = 23) HV-P (n = 24) P F GRS/% 14.5 ± 6.5***, ### 7.0 ± 2.7 34.2 ± 10.7^ 41.0 ± 6.5 < 0.001 153 GCS/% -11.1 ± 4.4***, ### -5.4 ± 2.2 -19.9 ± 2.8^^^ -24.7 ± 2.0 < 0.001 185.6 GLS/% -7.7 ± 3.2**, ### -4.3 ± 1.7 -13.6 ± 4.1 -15.8 ± 1.5 < 0.001 101.4 GRS: global radial strain; GCS: global circumferential strain; GLS: global longitudinal strain. The other abbreviations are explained in the notes to Fig 1. ** P < 0.01, *** P < 0.05, vs. DCM-P; ### P < 0.001, vs. HV-H; ^ P < 0.05, ^^^ P < 0.001, vs. HV-P. The data are expressed as $ \bar{x} \pm s $. All parameters are analyzed by Welch's test. 2.3 高海拔DCM患者心肌应变与心功能参数的关系
见表4。LVEF、LVSV与GRS、GCS绝对值呈正相关。LVSV与GLS绝对值呈正相关。
表 4 高海拔DCM患者心功能与心肌应变的相关性Table 4. Relationship between cardiac function and myocardial strain in patients with DCM at a high altitudeParameter GRS/% (n = 29) GCS/% (n = 29) GLS/% (n = 29) r P r P r P LVEF/% 0.533 0.003 0.486 0.009 0.319 0.098 LVEDV/mL -0.237 0.225 -0.119 0.546 -0.011 0.954 LVESV/mL -0.347 0.070 -0.225 0.249 -0.101 0.610 LVSV/mL 0.558 0.002 0.536 0.003 0.452 0.016 All abbreviations are explained in the notes to Table 2 and Table 3. 3. 讨论
DCM的临床病程具有高度异质性,从无明显临床症状到严重心力衰竭,甚至心脏猝死,左心室舒张收缩功能障碍是DCM的主要病理生理改变[13-15]。DCM不良重构主要表现为左室壁变薄和扩张、左室充盈压力增加、心室顺应性降低[5]。已有研究发现DCM患者LVEDV和LVESV均增加,而LVEF降低[16-17],但高海拔DCM患者与平原DCM患者二者是否存在差异未见文献报道。本研究对比高海拔DCM患者与高海拔志愿者的心功能参数,发现高海拔DCM患者LVEDV、LVESV高于健康志愿者,LVEF、LVSV低于健康志愿者,与平原DCM结果一致。
对于海拔
2500 m 以上的高海拔地区,低压低氧导致肺泡氧分压及肺静脉内血氧分压下降,机体器官、组织、细胞水平获得的氧气均减少,人体将通过神经及体液调节氧气供需平衡[18-20]。长期居住在高海拔地区的人群通过代偿性低氧调节,逐步恢复机体稳态,维持其生存能力,最终适应高海拔环境[8, 21-22]。李慧兰等[23]发现高海拔急下平原的受试者比世居平原受试者的LVEDV、LVESV高,本研究在平原检查的高海拔健康志愿者LVEDV、LVESV也高于世居平原的健康志愿者。但是高海拔DCM患者心功能与平原DCM患者没有明显差异,这可能与机体的长期低压低氧适应性反应有关。CMR-FT技术在测量心肌应变中具有广泛的临床应用前景。这种方法不需要进行额外序列的扫描,使用常规电影CMR图像,经过后处理即可获得心肌应变,易于临床实践中应用[24-25]。既往研究已证实了CMR-FT的可行性和有效性,多个应变参数显示了对于DCM患者的诊断价值[26-27]。有学者发现DCM主要累及心肌的中层和外层,表现为周向心肌应变的降低[6, 28],本研究与既往研究一致,高海拔DCM患者的GCS比高海拔健康志愿者低。此外,既往研究发现不仅GCS降低,GRS、GLS也降低[16-17],本研究也发现高海拔DCM患者的GRS和GLS均降低。本研究还发现高海拔健康志愿者的GRS、GCS均比平原健康志愿者低,提示高海拔低压低氧环境下心肌应变可能降低。值得一提的是高海拔DCM患者的GRS、GCS、GLS反而比平原DCM患者高,表明高海拔DCM患者心肌应变的改变可能比平原DCM小,其中原因有待于进一步研究,可能与心脏在长期低压低氧环境下,其心肌耐受性更强有关系。虽然高海拔DCM患者心肌应变比平原DCM患者改变小,且心肌应变与心功能成正比,但是最终二者的心功能无差异,说明心肌应变比心功能更能显示高海拔地区与平原地区的差异,需要进一步通过大样本临床研究验证和基础研究来探究其原理。
本研究存在以下不足:第一,高海拔地区患者样本量较小,今后需要长期且更大的样本量进一步验证相关结果。第二,本研究比较了高海拔DCM患者与平原DCM患者心肌应变的差异,作为回顾性研究,没有办法通过自身对照,对高海拔DCM、平原DCM患者生病前后心功能及心肌应变的变化进行比较,今后需要前瞻性研究进一步比较。第三,本研究虽然匹配了年龄、性别等因素,但仍需进一步研究其他因素对结果的影响。且高海拔DCM与平原DCM心肌应变存在差异,原因尚不明确,需要更深入地研究其存在的机制。第四,CMR-FT技术依赖于不同厂家的磁共振、不同的第三方后处理软件,结果的一致性需要指南和共识声明明确参考标准。
综上所述,本研究显示CMR-FT能够定量评估高海拔DCM患者的心肌应变,发现高海拔地区DCM患者与平原DCM患者心肌应变有差异,为临床个性化治疗DCM患者,改善患者预后提供影像学依据。
* * *
作者贡献声明 王哲涛负责论文构思、经费获取、研究方法和初稿写作,王春华负责经费获取和研究项目管理,尹红科负责调查研究,赵思斯和索靖航负责数据审编,王磊负责正式分析,陈榆舒负责经费获取和验证,周鹏负责监督指导,郜发宝负责经费获取、提供资源和审读与编辑写作。所有作者已经同意将文章提交给本刊,且对将要发表的版本进行最终定稿,并同意对工作的所有方面负责。
Author Contribution WANG Zhetao is responsible for conceptualization, funding acquisition, methodology, and writing--original draft. WANG Chunhua is responsible for funding acquisition and project administration. YIN Hongke is responsible for investigation. ZHAO Sisi and SUO Jinghang are responsible for data curation. WANG Lei is responsible for formal analysis. CHEN Yushu is responsible for funding acquisition and validation. ZHOU Peng is responsible for supervision. GAO Fabao is responsible for funding acquisition, resources, and writing--review and editing. All authors consented to the submission of the article to the Journal. All authors approved the final version to be published and agreed to take responsibility for all aspects of the work.
利益冲突 所有作者均声明不存在利益冲突
Declaration of Conflicting Interests All authors declare no competing interests.
-
图 1 舒张期与收缩期CMR图像及心内外膜勾画
Figure 1. Diastolic and systolic CMR images and outlining of endocardium and epicardium
DCM-H: patient with dilated cardiomyopathy living at a high altitude; DCM-P: patient with dilated cardiomyopathy in low-altitude plain regions; HV-H: healthy volunteer living at a high altitude; HV-P: healthy volunteer in low-altitude plain regions. The green line traces the epicardium, and the red line marks the endocardium.
表 1 受试者基本资料
Table 1 Basic data of the subjects
Variable DCM-H (n = 29) DCM-P (n = 27) HV-H (n = 23) HV-P (n = 24) P F Age/yr. 42.2 ± 13.2 44.2 ± 13.2 38.8 ± 10.9 44.3 ± 14.5 0.433 0.921 Male/case (%) 19 (65.5) 17 (63.0) 12 (52.2) 13 (54.2) 0.715 1.359 Body mass/kg 66.8 ± 16.0 66.9 ± 10.3 63.4 ± 15.0 66.6 ± 9.7 0.27 1.344 Height/cm 166.1 ± 7.2 164.6 ± 9.1 166.0 ± 10.7 163.0 ± 8.9 0.589 0.644 SBP/mmHg 112.0 ± 20.9## 111.5 ± 19.4 129.5 ± 6.8^ 115.0 ± 14.9 < 0.001 14.365 DBP/mmHg 72.3 ± 15.6## 74.9 ± 11.8 84.8 ± 5.7^^^ 76.0 ± 9.1 0.001 12.000 HR/min-1 77.7 ± 15.6*, ## 91.5 ± 19.3 91.8 ± 8.6 85.3 ± 9.1 0.001 6.245 SBP: systolic blood pressure; DBP: diastolic blood pressure; HR: heart rate; the other abbreviations are explained in the notes to Fig 1. * P < 0.05, vs. DCM-P; ## P < 0.01, vs. HV-H; ^ P < 0.05, ^^^ P < 0.001, vs. HV-P. The data are expressed as $ \bar{x} \pm s$ except those for sex. 1 mmHg = 0.133 kPa. All the variables are analyzed by Welch's test except for body mass, which is analyzed by one-way ANOVA. 表 2 受试者心功能参数
Table 2 Cardiac function parameters of the subjects
Parameter DCM-H (n = 29) DCM-P (n = 27) HV-H (n = 23) HV-P (n = 24) P F LVEF/% 25.5 ± 11.7### 18.4 ± 3.8 61.2 ± 6.0 64.3 ± 5.2 < 0.001 300.8 LVEDV/mL 303.2 ± 96.8### 329.1 ± 43.7 145.6 ± 34^^^ 85.1 ± 20.3 < 0.001 268.7 LVESV/mL 231.6 ± 101.9### 268.9 ± 34.7 59.3 ± 25.7^^^ 32.3 ± 11.4 < 0.001 327.5 LVSV/mL 71.6 ± 18.2## 60.3 ± 21.7 86.3 ± 13.2^^^ 52.8 ± 14.6 < 0.001 26.8 LVEF: left ventricular ejection fraction; LVEDV: left ventricle end-diastolic volume; LVESV: left ventricle end-systolic volume; LVSV: left ventricle stroke volume. The other abbreviations are explained in the notes to Fig 1. ## P < 0.01, ### P < 0.001, vs. HV-H; ^^^ P < 0.001, vs. HV-P. The data are expressed as $ \bar{x} \pm s$. All parameters are analyzed by Welch's test. 表 3 受试者心肌应变参数
Table 3 Myocardial strain of parameters the subjects
Parameter DCM-H (n = 29) DCM-P (n = 27) HV-H (n = 23) HV-P (n = 24) P F GRS/% 14.5 ± 6.5***, ### 7.0 ± 2.7 34.2 ± 10.7^ 41.0 ± 6.5 < 0.001 153 GCS/% -11.1 ± 4.4***, ### -5.4 ± 2.2 -19.9 ± 2.8^^^ -24.7 ± 2.0 < 0.001 185.6 GLS/% -7.7 ± 3.2**, ### -4.3 ± 1.7 -13.6 ± 4.1 -15.8 ± 1.5 < 0.001 101.4 GRS: global radial strain; GCS: global circumferential strain; GLS: global longitudinal strain. The other abbreviations are explained in the notes to Fig 1. ** P < 0.01, *** P < 0.05, vs. DCM-P; ### P < 0.001, vs. HV-H; ^ P < 0.05, ^^^ P < 0.001, vs. HV-P. The data are expressed as $ \bar{x} \pm s $. All parameters are analyzed by Welch's test. 表 4 高海拔DCM患者心功能与心肌应变的相关性
Table 4 Relationship between cardiac function and myocardial strain in patients with DCM at a high altitude
Parameter GRS/% (n = 29) GCS/% (n = 29) GLS/% (n = 29) r P r P r P LVEF/% 0.533 0.003 0.486 0.009 0.319 0.098 LVEDV/mL -0.237 0.225 -0.119 0.546 -0.011 0.954 LVESV/mL -0.347 0.070 -0.225 0.249 -0.101 0.610 LVSV/mL 0.558 0.002 0.536 0.003 0.452 0.016 All abbreviations are explained in the notes to Table 2 and Table 3. -
[1] PINTO Y M, ELLIOTT P M, ARBUSTINI E, et al. Proposal for a revised definition of dilated cardiomyopathy, hypokinetic non-dilated cardiomyopathy, and its implications for clinical practice: a position statement of the ESC working group on myocardial and pericardial diseases. Eur Heart J, 2016, 37(23): 1850-1858. doi: 10.1093/eurheartj/ehv727.
[2] 王哲涛, 任静, 周鹏, 等. 心脏磁共振影像组学在非缺血性心肌病中的应用研究进展. 广西医学, 2024, 46(2): 204-209. doi: 10.11675/j.issn.0253-4304.2024.02.05. WANG Z T, REN J, ZHOU P, et al. Research advances in the application of cardiac magnetic resonance radiomics in non-ischemic cardiomyopathy. Guangxi Medical Journal, 2024, 46(2): 204-209. doi: 10.11675/j.issn.0253-4304.2024.02.05.
[3] MILITARU S, PANOVSKY R, HANET V, et al. Multivendor comparison of global and regional 2D cardiovascular magnetic resonance feature tracking strains vs tissue tagging at 3T. J Cardiovasc Magn Reson, 2021, 23(1): 54. doi: 10.1186/s12968-021-00742-3.
[4] RAJIAH P S, KUMAR V, DOMENECH-XIMENOS B, et al. Utility of MRI and CT in sports cardiology. Radiographics, 2025, 45(3): e240045. doi: 10.1148/rg.240045.
[5] XIANG X, SONG Y, ZHAO K, et al. Incremental prognostic value of left atrial and biventricular feature tracking in dilated cardiomyopathy: a long-term study. J Cardiovasc Magn Reson, 2023, 25(1): 76. doi: 10.1186/s12968-023-00967-4.
[6] ZHU L, WU J, HAO X, et al. Value of cardiac magnetic resonance feature tracking technology in the differential diagnosis of isolated left ventricular noncompaction and dilated cardiomyopathy. Quant Imaging Med Surg, 2023, 13(3): 1453-1463. doi: 10.21037/qims-22-710.
[7] 何宗钊, 马四清, 邓莉, 等. 高海拔地区(4100 m)不同健康人群微循环特征及其体液因子的变化. 生理学报, 2021, 73(6): 917-925. doi: 10.13294/j.aps.2021.0092. HE Z Z, MA S Q, DENG L, et al. Microcirculation characteristics and humoral factors of healthy people from different populations at high altitude (4 100 m). Acta Physiologica Sinica, 2021, 73(6): 917–925. doi: 10.13294/j.aps.2021.0092.
[8] 吴岑岑, 蔡嘉庚, 蔡珠兰, 等. 世居平原人群高海拔环境暴露后心血管系统生理适应性变化. 中国医学前沿杂志(电子版), 2024, 16(3): 67-71. doi: 10.12037/YXQY.2024.03-12. WU C C, CAI J G, CAI Z L, et al. Physiological acclimatization of the cardiovascular system in plains-dwelling population after high-altitude environment exposure. Chin J Front Med Sci (E Version), 2024, 16(3): 67-71. doi: 10.12037/YXQY.2024.03-12.
[9] CHEN C, LI B, CHEN H, et al. Epigallocatechin-3-gallate ameliorated iron accumulation and apoptosis and promoted neuronal regeneration and memory/cognitive functions in the hippocampus induced by exposure to a chronic high-altitude hypoxia environment. Neurochem Res, 2022, 47(8): 2254-2262. doi: 10.1007/s11064-022-03611-2.
[10] FANG X, JI Y, LI S, et al. Paeoniflorin attenuates cuproptosis and ameliorates left ventricular remodeling after AMI in hypobaric hypoxia environments. J Nat Med, 2024, 78(3): 664-676. doi: 10.1007/s11418-024-01781-7.
[11] CHEN H, CHEN C, QIN Y, et al. Protective effects of epigallocatechin-3-gallate counteracting the chronic hypobaric hypoxia-induced myocardial injury in plain-grown rats at high altitude. Cell Stress Chaperones, 2023, 28(6): 921-933. doi: 10.1007/s12192-023-01386-1.
[12] BOZKURT B, COLVIN M, COOK J, et al. Current diagnostic and treatment strategies for specific dilated cardiomyopathies: a scientific statement from the American Heart Association. Circulation, 2016, 134(23): e579-e646. doi: 10.1161/CIR.0000000000000455.
[13] GORCSAN J, EGUCHI S. Predictors of arrhythmic outcomes in patients with dilated and nondilated left ventricular cardiomyopathies. J Am Coll Cardiol, 2024, 83(19): 1852-1854. doi: 10.1016/j.jacc.2024.03.404.
[14] ZHOU Y, XU Y, LI Y, et al. Late gadolinium-enhanced cardiac magnetic resonance for predicting left ventricular reverse remodeling in dilated cardiomyopathy a comprehensive review and meta-analysis. J Cardiovasc Magn Reson, 2025: 101860. doi: 10.1016/j.jocmr.2025.101860.
[15] DATTANI A, MARROW B A, GULSIN G S, et al. Association between coronary microvascular dysfunction and exercise capacity in dilated cardiomyopathy. J Cardiovasc Magn Reson, 2024, 26(2): 101108. doi: 10.1016/j.jocmr.2024.101108.
[16] STEEN H, GIUSCA S, MONTENBRUCK M, et al. Left and right ventricular strain using fast strain-encoded cardiovascular magnetic resonance for the diagnostic classification of patients with chronic non-ischemic heart failure due to dilated, hypertrophic cardiomyopathy or cardiac amyloidosis. J Cardiovasc Magn Reson, 2021, 23(1): 45. doi: 10.1186/s12968-021-00711-w.
[17] GAO Y, WANG H P, LIU M X, et al. Early detection of myocardial fibrosis in cardiomyopathy in the absence of late enhancement: role of T1 mapping and extracellular volume analysis. Eur Radiol, 2023, 33(3): 1982-1991. doi: 10.1007/s00330-022-09147-x.
[18] 颜春龙, 马金凤, 齐先龙, 等. 3.0 T MRI对高原与平原地区健康正常人心脏结构及功能的对比研究. 磁共振成像, 2020, 11(7): 526-530. doi: 10.12015/issn.1674-8034.2020.07.010. YAN C L, MA J F, QI X L, et al. A comparative study of 3.0 tesla cardiac magnetic resonance imaging on cardiac structure and function of healthy normal people in plateau and plain areas. Chin J Magn Reson Imaging, 2020, 11(7): 526-530. doi: 10.12015/issn.1674-8034.2020.07.010.
[19] SUN Y, ZHANG C, TIAN D, et al. Application of 7. 0 T ultra-high-field MRI in evaluating the structure and function of the right ventricle of the heart in rats under a chronic hypoxic environment at high altitude. Ann Transl Med, 2021, 9(20): 1585. doi: 10.21037/atm-21-5078.
[20] ZHANG M, ZHU D, WAN Y, et al. Using 7. 0 T cardiac magnetic resonance to investigate the effect of estradiol on biventricular structure and function of ovariectomized rats exposed to chronic hypobaric hypoxia at high altitude. Arch Biochem Biophys, 2022, 725: 109294. doi: 10.1016/j.abb.2022.109294.
[21] 郝艳, 雷富民. 适应性演化的分子遗传机制: 以高海拔适应为例. 遗传, 2022, 44(8): 635-653. doi: 10.16288/j.yczz.22-108. HAO Y, LEI F M. Genetic mechanism of adaptive evolution: the example of adaptation to high altitudes. Hereditas(Beijing), 2022, 44(8): 635-653. doi: 10.16288/j.yczz.22-108.
[22] 张剑搏, 丁学智, AHMAD A A, 等. 高原土著动物适应性进化的研究进展. 畜牧兽医学报, 2019, 50(9): 1723-1736. doi: 10.11843/j.issn.0366-6964.2019.09.001. ZHANG J B, DING X Z, AHMAD A A, et al. Advances in research on adaptive evolution of native animals of tibetan plateau. Acta Veterinaria et Zootechnica Sinica, 2019, 50(9): 1723-1736. doi: 10.11843/j.issn.0366-6964.2019.09.001.
[23] 李慧兰, 陈小龙, 罗韬, 等. 基于心脏磁共振的高原与平原患者心脏结构与功能对比分析教学研究. 中国医学影像学杂志, 2022, 30(12): 1241-1246. doi: 10.3969/j.issn.1005-5185.2022.12.008. LI H L, CHEN X L, LUO T, et al. Comparative analysis of cardiac structure and function between high-altitude and plain patients based on cardiac magnetic resonance: a teaching study. Chin J Med Imaging, 2022, 30(12): 1241-1246. doi: 10.3969/j.issn.1005-5185.2022.12.008.
[24] GAO Y, PU C, LI Q, et al. Assessment of right atrial function measured with cardiac MRI feature tracking for predicting outcomes in patients with dilated cardiomyopathy. Radiology, 2024, 310(3): e232388. doi: 10.1148/radiol.232388.
[25] OCHS A, RIFFEL J, OCHS M M, et al. Myocardial mechanics in dilated cardiomyopathy: prognostic value of left ventricular torsion and strain. J Cardiovasc Magn Reson, 2021, 23(1): 136. doi: 10.1186/s12968-021-00829-x.
[26] MA H Y, XIE G Y, TAO J, et al. Identification of patients with nonischemic dilated cardiomyopathy at risk of malignant ventricular arrhythmias: insights from cardiac magnetic resonance feature tracking. BMC Cardiovasc Disord, 2024, 24(1): 29. doi: 10.1186/s12872-023-03655-4.
[27] GAO Y, SHI J, SHI Y, et al. Feasibility and reproducibility of cardiovascular magnetic resonance-feature tracking for quantitative right atrial function in dilated cardiomyopathy patients. Quant Imaging Med Surg, 2024, 14(5): 3312-3325. doi: 10.21037/qims-23-1119.
[28] ZHENG T, MA X, LI S, et al. Value of cardiac magnetic resonance fractal analysis combined with myocardial strain in discriminating isolated left ventricular noncompaction and dilated cardiomyopathy. J Magn Reson Imaging, 2019, 50(1): 153-163. doi: 10.1002/jmri.26616.

开放获取 本文遵循知识共享署名—非商业性使用4.0国际许可协议(CC BY-NC 4.0),允许第三方对本刊发表的论文自由共享(即在任何媒介以任何形式复制、发行原文)、演绎(即修改、转换或以原文为基础进行创作),必须给出适当的署名,提供指向本文许可协议的链接,同时标明是否对原文作了修改;不得将本文用于商业目的。CC BY-NC 4.0许可协议详情请访问 https://creativecommons.org/licenses/by-nc/4.0

 首页
首页


 下载:
下载: